Researchers from the University of Texas have found an immunosuppressing target for the treatment of glioblastoma. In mice studies the team has identified CD73 macrophages which could be used to treat the cancers. The team also performed studies on human tumours to arrive at their conclusions. The study was published in the latest issue of the journal Nature Medicine this week.
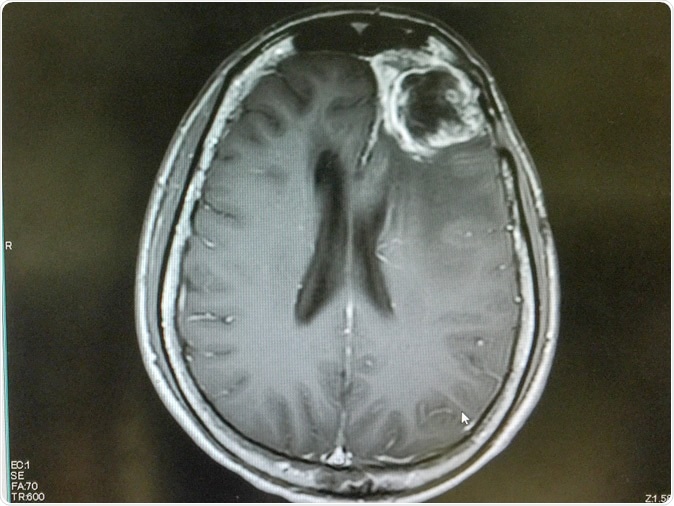
MRI of brain showing left frontal gliblastoma. Image Credit: O_Akira / Shutterstock
Glioblastoma is one of the most aggressive forms of brain cancer that is primary in nature and affects special cells of the brain called glioma. Treatment for this aggressive cancer is often difficult and surgery as well as radiation therapy often fails to cure this cancer. This cancer is usually fast growing and there may be no symptoms of the cancer in initial stages. The symptoms may appear only when the cancer is larger and more difficult to treat. At later stages brain functions are abnormal and with rapid tumour growth the condition soon becomes fatal. In some patients initial treatment may help slow the progress of the disease temporarily but in most patients there is return of the cancer followed by its aggressive relapse and growth.
For this study the team from University of Texas MD Anderson Cancer Center worked with immune macrophages that contain high amounts of CD73 that are capable of killing the tumour cells using a “anti-PD-1 checkpoint blockade”. These macrophages contain high levels of surface enzyme called CD73 and these unique macrophages are commonly seen associated with glioblastomas. First author of the study, Dr. Sangeeta Goswami, assistant professor of Genitourinary Medical Oncology said, “By studying the immune microenvironments across tumor types, we've identified a rational combination therapy for glioblastoma.”
As the first part of their study the team used human tumours and found the CD73 expressing macrophages associated with these tumours. They also noted that increased presence of these cells within the tumours reduced the chances of survival in the patients.
For this study the team found immune cells in five different types of tumours using CyTOF mass cytometry and single-cell RNA sequencing. They looked for the CD73-positive macrophages in this project. For this the team looked at 94 samples of human glioblastoma tumours, non-small cell lung cancers, cancers of prostate, cancers of kidney and colorectal cancers. In each of the cancers, they looked at the immune cells around the tumours. In the 13 samples of glioblastoma, they noted that more number of CD73 positive cells meant shorter survival in the patients. Macrophages that showed most number of CD68 also showed high levels of CD73 they noted. In nine more samples of glioblastomas, this theory was proved to be correct.
Next they combined two types of immunotherapies called the anti-PD-1 and anti-CTLA-4 immunotherapies in mice that were deficient of CD73 by genetic tweaking. These mice without the CD73 containing macrophages were called CD73 knockout mice. When the combined immunotherapy was tried upon mice without the CD73 containing macrophages, the tumour growth among them was halted and the survival in the mice increased. Dr. Padmanee Sharma, professor of Genitourinary Medical Oncology and Immunology, an author of the study said, “We're working with pharmaceutical companies that are developing agents to target CD73 to move forward with a glioblastoma clinical trial in combination with anti-PD-1 and anti-CTLA-4 checkpoint inhibitors.”
The team then identified a gene signature for the cells with CD73 using RNA sequencing, based on their findings and from a library of 525 glioblastoma samples preserved in the Cancer Genome Atlas, they matched their findings. The results of the immune cells in the tumour again correlated with the decreased survival.
As a next step they used CyTOF mass cytometry cluster analysis on the five samples of glioblastoma tumours that had been treated with PD-1 checkpoint inhibitor pembrolizumab and compared them with seven samples that had not been treated with these drugs. Despite pembrolizumab treatment, three cancers persisted as did the CD73 expressing macrophasges. This also reduced the lifespan, they noted. The team thus could conclude that those having CD73 expressing macrophages showed poorer responses to available medications and had a poorer clinical outcome.
In the mice treated with PD-1 inhibitors or a combination of PD-1 and CTLA-4 immune checkpoint inhibitors, those mice with CD73 and treatment survived longer than those without treatment. Those who had their CD73 knocked out genetically had even longer survival if they were treated with the medications, the team concluded. Anti-PD-1 alone however did not prove to be beneficial.
The authors of the study wrote in conclusion, “Based on our data and earlier studies, we propose a combination therapy strategy to target CD73 plus dual blockade of PD-1 and CTLA-4.”
The team explained that most studies begin in lab animals and once theories are proven, the researchers work on human tissues. For this study, the process was reverse and this is called “reverse translation”. For this study the team looked at human tumours and analysed them first before testing the hypothesis in mice. If successful, the combination immunotherapy could be used for treatment of the cancer. Sharma explained that this study could also be extended to other cancers once scientists are better aware of the microenvironments of the tumours and the immune cells that they contain. She added that these immune environments and their interactions may differ from cancer to cancer. She said, “Understanding what's different in immune niches across cancers provides clues and targets for treating tumours. That's why we did this study.”
Journal reference:
Goswami, S., Walle, T., Cornish, A.E. et al. Immune profiling of human tumors identifies CD73 as a combinatorial target in glioblastoma. Nat Med (2019) doi:10.1038/s41591-019-0694-x, https://www.nature.com/articles/s41591-019-0694-x