A new study published in the journal Pediatrics shows that children with spina bifida, a congenital spinal disorder, who had corrective surgery in the womb, show significantly more benefit than those whose operations were performed after birth, even a decade later. These children have more of a chance to walk by themselves and a lower risk of needing more surgeries, compared to those whose condition is corrected only after birth.
Spina bifida
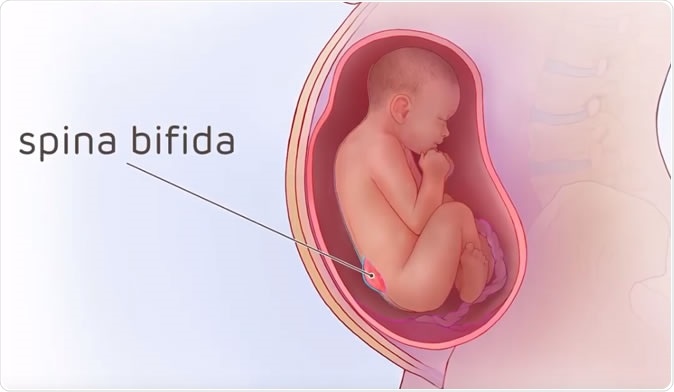
Spina bifida is the term for the birth defect that occurs due to the failure of the spinal column to form completely around the spinal cord, leaving part of it open to the outside. This means the child is at risk of infection of the spinal meninges, injury to the nerves, bowel or bladder defects, and weakness or paralysis below the site of the defect. It affects about 1 in 1,500 children.
Spina bifida Illustrated - Credit: The Children's Hospital of Philadelphia
The most severe form of this is the meningomyelocele, when the spinal cord as well as the coverings over it bulge out through the defective part, which appears as an opening in the spinal column. If this protrusion is large enough it can cause a block to the flow of the cerebrospinal fluid. This can also draw the whole spinal cord downwards, and thus pull the lowest part of the brain into the opening at the base of the skull, which is called hindbrain herniation.
Spina Bifida Medical Animation | Cincinnati Fetal Center
What is known
Traditional fetal surgery in spina bifida is meant to correct meningomyelocele. A landmark earlier study in 2011 showed conclusively that fetal surgery was associated with better outcomes by 12 months after birth, in terms of fewer operations required to shunt blocked cerebrospinal fluid away from the brain. By 30 months of age, the children who had undergone fetal surgery were more likely to walk without having to use assistive devices like crutches.
The current MOMS2 study was meant to continue the evaluation of these children. It included 161 children, of whom 79 had undergone fetal surgery and 82 had conventional surgery. It was carried out at the same 3 centers that took place in the first MOMS trial, and consisted of one complete assessment carried out between June 2011 and April 2017 on all the children, who were at the age of 6 years to 10 years by then. This included neurologic and developmental testing, physical examination, functioning tests, and a questionnaire to evaluate independent living skills.
The findings
Children who had surgery before birth had a 93% chance of walking unaided by school age compared to 80% in the traditional surgery group. The percentage of children in the first and second groups who needed further surgery to place a shunt in the brain to relieve fluid accumulation in the brain (a condition called hydrocephalus) was 49% and 85% respectively. Shunt replacements were required by 47% and 70% of children in the first and second groups, respectively. A motor skill assessment also showed that the first group had on average higher scores.
The children in the first group were almost 6 times more likely to be able to visit the bathroom on their own compared to those operated on after birth, which shows their far better degree of bladder and bowel control. The number of catheterizations required was less in the first group. Quality of life was superior for both the children and their families, and overall stress levels were reduced, in the first group.
Parameters which are not significantly affected by prenatal vs postnatal surgery include independent living skills, including communication skills, skills of daily living and social skills.
Implications
Co-author N. Scott Adzick describes his reaction to the findings: “It is extremely gratifying to see that the positive results from the initial MOMS trial endure into childhood. Fetal surgery is a complex and serious procedure and should only be done by experienced teams. Research needs to continue to refine the technique in a way that will improve outcomes even further."
Researcher Menachem Miodovnik sums up the implications of this study: “Prenatal surgery for myelomeningocele carries benefits and risks, compared to traditional postnatal surgery. This study provides important information for physicians with patients who are considering prenatal surgery.” Adzick goes on to say: “These findings add to the growing body of literature demonstrating the benefits of prenatal surgery for spina bifida. Providers should take these findings into account when counseling expectant mothers to ensure that families considering prenatal surgery for their fetus understand the potential risks and benefits.”
At present, the fetal surgery for meningomyelocele at centers of excellence has continued to improve technically, becoming shorter while the pregnancy continues for longer after the intrauterine procedure, preventing many preterm births.
Journal reference:
Houtrow AJ, Thom EA, Fletcher JM, Burrows PK, Adzick NS, Thomas NH, Brock III JW, Cooper T, Lee H, Bilaniuk L, Glenn OA, Pruthi S, MacPherson C, Farmer DL, Johnson MP, Howell LJ, Gupta N, Walker WO. "Prenatal Repair of Myelomeningocele and School-Age Functional Outcomes," Pediatrics, online January 24, 2020. https://pediatrics.aappublications.org/content/145/2/e20191544