Despite its critical role in saving lives, over 5 billion people lack access to safe, affordable medical oxygen—this report outlines the urgent reforms needed to bridge the gap.
 Study: Reducing global inequities in medical oxygen access: the Lancet Global Health Commission on medical oxygen security. Image Credit: AlteredR / Shutterstock
Study: Reducing global inequities in medical oxygen access: the Lancet Global Health Commission on medical oxygen security. Image Credit: AlteredR / Shutterstock
Medical oxygen is an essential clinical need for children and adults with a range of acute and chronic conditions, as well as for those undergoing surgery. Although medical oxygen must be available to everyone in need, the real-world scenario points to long-standing inequities in access to this vital public health system.
The Lancet Global Health Commission on Medical Oxygen Security was launched in 2022 to understand the root causes of medical oxygen shortages and produce comprehensive and actionable recommendations for governments, industry, global health agencies, donors, the healthcare workforce, and researchers. The commission emphasizes that medical oxygen is not just a commodity but an essential public service requiring coordinated investments in production, distribution, regulation, and financing.
A recent report published in The Lancet Global Health provides key findings from the commission on medical oxygen security.
The global need for medical oxygen
About 374 million people need medical oxygen globally each year. About 82% of them live in low-income and middle-income countries. With increasing population growth and unmet surgery and long-term oxygen therapy needs, the demand for medical oxygen is rising globally. In addition to acute medical needs, an estimated 9.2 million people with chronic obstructive pulmonary disease (COPD) require long-term oxygen therapy (LTOT) annually, yet access to LTOT remains nearly nonexistent in many low-resource settings.
The key steps to reduce oxygen need include immunization, smoking cessation, air pollution control, nutritional improvements, and climate change mitigation. The commission also highlights that public health interventions, such as increasing pneumococcal and respiratory syncytial virus (RSV) vaccine coverage, can significantly reduce the incidence of respiratory infections and lessen oxygen demand.
The demand for oxygen can increase substantially during emergencies, such as epidemics, pandemics, natural disasters, and war. During the coronavirus disease 2019 (COVID-19) pandemic, an additional 52 million patients needed 1.9 billion Nm³ of oxygen to treat the disease worldwide. This surge in demand severely overwhelmed health systems in many low-resource countries, where an estimated 45% of COVID-19 patients in intensive care units never received oxygen therapy.
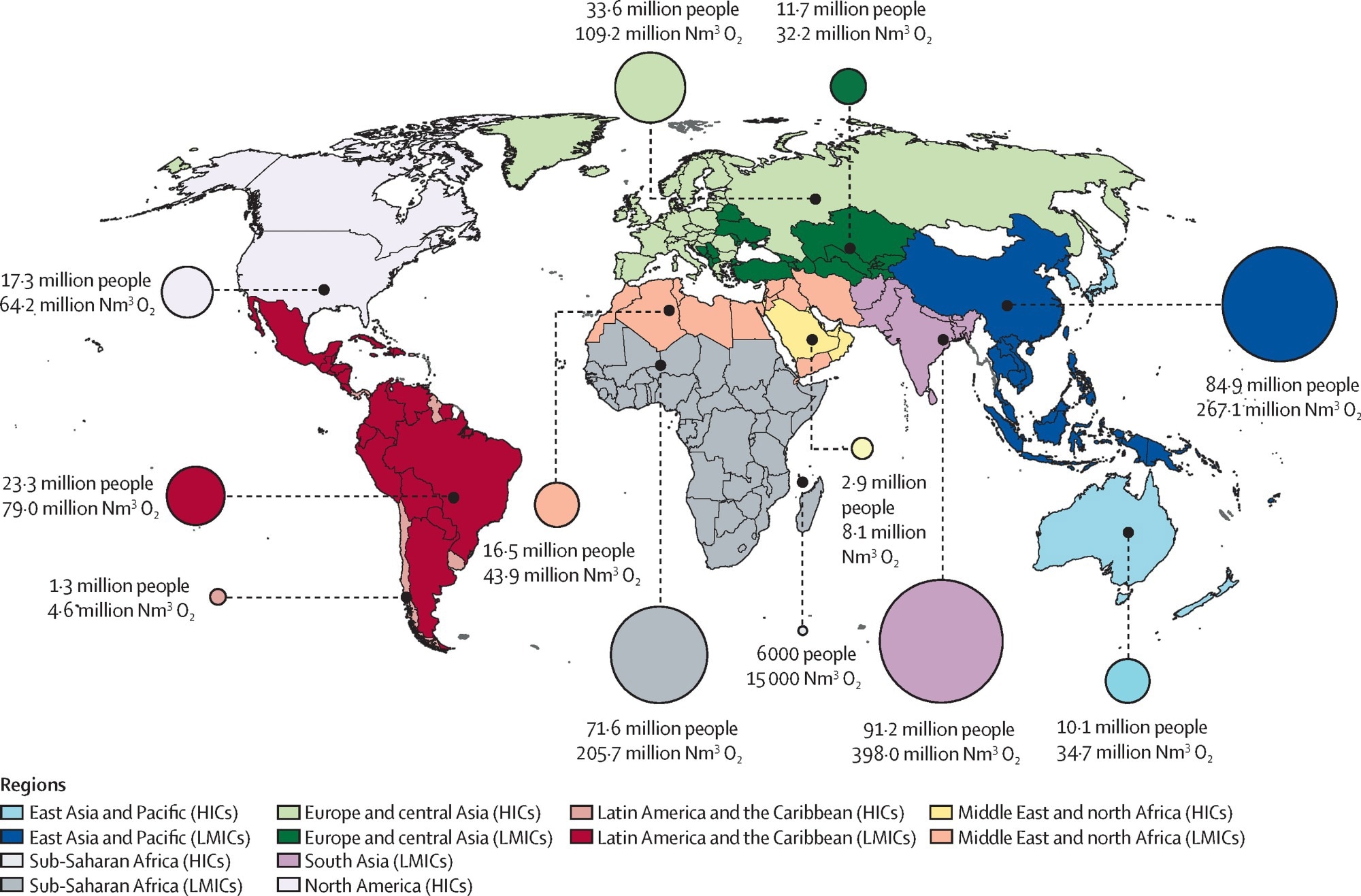
Location of people with acute medical and surgical oxygen needs in 2021, and minimum volume of oxygen required to meet need, by World Bank region Note that this figure excludes oxygen requirements related to COVID-19. Oxygen need is represented by the circles, the sizes of which are proportional to the number of people in that region who need medical oxygen therapy. Minimum volume of oxygen required to meet need was calculated using data for recommended and usual flow rates and duration for various conditions and assumes no inefficiencies in oxygen use and no wastage or inefficiencies in upstream oxygen production, supply, and distribution. HICs=high-income countries. LMICs=low-income and middle-income countries. Nm3=normal cubic metres.
Inequities in access to medical oxygen
There has been a massive shortage of medical oxygen supply in many low- and middle-income countries despite investments since the COVID-19 pandemic. More than 5 billion people—over 60% of the global population—lack access to safe, clinical-quality, and affordable oxygen services.
In low- and middle-income countries, sufficient oxygen therapy is available for only 30% of the people who need medical oxygen for acute or surgical conditions. The oxygen shortage is highest in sub-Saharan Africa, where only 9% of patients who need medical oxygen actually receive it.
Key factors contributing to such shortages include lack of essential oxygen service capacity in healthcare facilities, failure to understand the need for oxygen due to unavailability of testing instruments (pulse oximeter), lack of people visiting healthcare facilities, low-quality oxygen care, and high costs. Additionally, many healthcare facilities lack trained personnel to safely administer oxygen therapy, further exacerbating the crisis.
The cost of reducing oxygen shortage
An estimated $6.8 billion is required each year to overcome medical oxygen shortages in low- and middle-income countries. This estimate does not include the substantial costs of meeting the additional oxygen requirements caused by pandemics or costs for long-term oxygen therapy.
Although a considerable budget is required to overcome the shortage, oxygen therapy is as cost-effective as childhood vaccination. Investing in medical oxygen services would allow governments to achieve the Sustainable Development Goals and reduce mortality during future pandemics.
So far, national oxygen plans have been developed in fewer than 30 countries. The commission encourages all governments to do so by 2030. These plans must go beyond simply increasing oxygen supply; they require integrating oxygen systems into national healthcare infrastructure, ensuring adequate training of clinical and engineering workforces, and establishing governance structures to oversee implementation.
Such plans can be developed through collaborations between public and private sectors involved in medical oxygen delivery, including the health, education, industry, energy, and transport sectors. Private sector engagement is particularly crucial, as the medical oxygen industry plays a key role in ensuring stable production, pricing transparency, and reliable distribution.
Oxygen systems should also be integrated into broader national health plans and pandemic preparedness and response strategies.
Importance of pulse oximetry
Pulse oximetry, which measures oxygen saturation in blood, must be available for all patients at all levels of healthcare facilities to assess the need for oxygen. However, only 19% of patients visiting general hospitals in low- and middle-income countries can access pulse oximetry. This lack of access contributes to missed diagnoses of hypoxaemia, delays in oxygen therapy, and increased mortality risk.
Pulse oximetry is the least common practice in primary care facilities, rural healthcare facilities, and sub-Saharan Africa. The commission highlights the urgent need to make high-quality, robust pulse oximeters more affordable for all populations, including people with darker skin and infants and young children. New global efforts, such as the introduction of standardized oxygen coverage indicators and a national Access to Medical Oxygen Scorecard, aim to improve monitoring and accountability in oxygen service delivery.
Making oxygen systems affordable for all
The commission advises governments to define priorities and optimize their systems to suit local conditions. A mixed-source oxygen supply, including liquid oxygen, oxygen plants, oxygen cylinders, and oxygen concentrators, can benefit most health systems and facilities.
National oxygen systems can be operationalized either by governments or by private sectors. However, governments should ensure that costs are not shifted to patients. The commission strongly urges governments to include pulse oximetry and oxygen services in universal health coverage schemes and to pursue other strategies to minimize user fees. This is particularly important because many families in LMICs face catastrophic out-of-pocket expenses for oxygen therapy, often forcing them to make impossible financial decisions.
Governments should ensure price transparency in medical oxygen markets and align oxygen quality-related national regulations with the updated WHO International Pharmacopoeia.
Global health agencies should regularly assess the progress of medical oxygen industries. They should also hold private-sector manufacturers accountable for equitable pricing and production targets, similar to how the pharmaceutical industry is regulated.
The commission advises that access to medical oxygen should be fully integrated into global pandemic preparedness and response architecture.
The commission also advises that global health agencies and donors should maintain oxygen access as a global health priority, including supporting the new Global Oxygen Alliance and replenishing The Global Fund to Fight AIDS, Tuberculosis, and Malaria with a strong oxygen-access mandate.
With a primary focus on equity and sustainability, the commission provides a path for maximizing medical oxygen accessibility at a global scale. According to the commission, national medical oxygen systems should be at the forefront of ensuring the long-term health and sustainability of people and the planet. Integrating energy-efficient oxygen technologies and local maintenance solutions can further enhance sustainability while reducing financial and environmental costs.
Journal reference:
- Graham, H. R., King, C., Rahman, A. E., Kitutu, F. E., Greenslade, L., Aqeel, M., Baker, T., De Magalhães Brito, L. F., Campbell, H., Czischke, K., English, M., Falade, A. G., Garcia, P. J., Gil, M., Graham, S. M., Gray, A. Z., Howie, S. R. C., Kissoon, N., Laxminarayan, R., . . . Ssengooba, F. (2025). Reducing global inequities in medical oxygen access: The Lancet Global Health Commission on medical oxygen security. The Lancet Global Health. DOI: 10.1016/S2214-109X(24)00496-0, https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(24)00496-0/fulltext