A new study from Finland, published in February 2020 in the Journal of the American Heart Association, shows that many patients allow unhealthy habits to linger or creep in even after starting medications for high blood pressure or blood cholesterol.
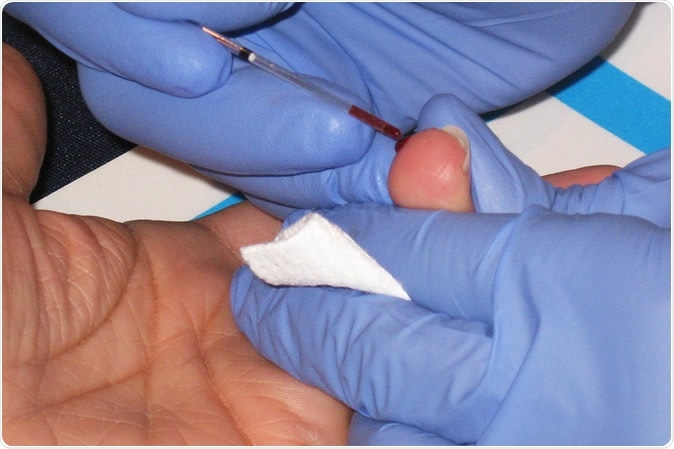
Cholesterol test - Drawing blood from the finger to use in a cholesterol test. Copyright American Heart Association
Medications for these conditions do not compensate for an unhealthy lifestyle, and people with either of these issues should begin lifestyle modifications such as appropriate physical activity, regular exercise, quitting smoking, and eating healthy foods in appropriate measures.
On the other hand, the study found that many people tried to control their blood pressure or blood lipid levels by lifestyle changes but stopped these health-promoting actions after they were started on prescription medications.
In fact, the current study found that the prescription of such drugs, in patients at high risk of cardiovascular disease (CVD), including heart disease and stroke, was associated with a higher chance of reduced physical activity and weight gain.
This points to the misperception prevalent among many people that medications to control a health issue are powerful enough to overcome even an unhealthy lifestyle and magically keep them healthy. Researcher Maarit J. Korhonen says, “Medication shouldn’t be viewed as a free-pass to continue or start an unhealthy lifestyle.”
The study
The current study was motivated by the desire to know if people on medications, who had health issues, were motivated to alter their lifestyles sufficiently to experience real benefit from the drugs. The researchers looked at over 40,000 people working in the public sector. Over 80% of them were females, with an average age of 52 years. None of them had a history of heart disease or stroke.
The researchers surveyed all participants at least twice at intervals of 4 years, over the period 2000 to 2013. There was a questionnaire administered at baseline as well as a follow-up questionnaire. The data included the BMI, physical activity, alcohol intake and whether the individual had smoked or was a smoker. Medication-related data was retrieved from the pharmacy to find out if these patients had been taking the prescribed drugs.
The participants were classified as those who started to take these drugs to prevent CVD at any time between the baseline and the next survey, and those who were not on medications during this period.
The findings
The scientists found that participants who began to take medications during this period had the following habit changes:
- An 8% higher chance of becoming less physically active: regular exercise has long been known to markedly lower the risk of CVD.
- An 82% higher chance of becoming heavier or obese: obesity increases the risk for diabetes, hypertension and CVD, among others.
- A 26% higher chance of giving up smoking: smoking is the cause of about a quarter of all deaths from CVD, that is, about 200,000 deaths a year. Among non-smokers, 33 000 die each year due to second-hand smoke-related CVD.
- Reduced alcohol intake: while alcohol raises the blood pressure and body weight, on average, it is also linked to a decreased overall risk for CVD as well as for death from CVD.
Quitting smoking can often be linked to an increase in body weight. On average, people may gain up to 5 kilograms, mostly over the first three months, and the rest over the next 5 years. However, the average weight gain of those participants who stopped smoking was more in those who started taking medications compared to those who didn’t.
Limitations and conclusions
The study didn’t include data on what the participants ate, their blood pressure, and cholesterol levels. Moreover, during the study period, extensive public health efforts were on to prevent and manage diabetes mellitus in Finland, where the survey took place. Therefore, some of the changes in the habits of the participants may have been prompted by this initiative.
Most of the participants were female and working in the public sector, and all were white.
These limitations make it more difficult to extrapolate the conclusions to other ethnic and racial groups, countries without good public health programs, and those where diabetes management and prevention is not a priority.
Nonetheless, Korhonen emphasizes, “People starting on medications should be encouraged to continue or start managing their weight, be physically active, manage alcohol consumption and quit smoking.”
Source:
Journal reference:
Lifestyle Changes in Relation to Initiation of Antihypertensive and Lipid‐Lowering Medication: A Cohort Study Maarit J. Korhonen PhD [email protected] , Jaana Pentti BSc , Juha Hartikainen MD, PhD , Jenni Ilomäki PhD , Soko Setoguchi MD, DrPH , Danny Liew PhD , Mika Kivimäki FMed Sci , and Jussi Vahtera MD, Ph, https://www.ahajournals.org/doi/full/10.1161/JAHA.119.014168