Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes. In 2018, there were over 200 million cases of malaria worldwide. Now, a team of researchers found evidence that the malaria parasite can detect a molecule released by approaching immune cells, using it to protect itself and evade the attack by the body’s immune system.
The discovery of how malaria parasites escape the attack of the immune system could open the doors for the development of new antimalarial drugs, which can prevent the parasites from detecting incoming immune cells. ‘
The study, which was published in the journal eLife Sciences and led by researchers at the Singapore Immunology Network (SIgN), and the Agency for Science, Technology, and Research’s (A*STAR) highlights formerly unknown reversible mechanisms the parasite can use to evade the immune system.
The immune system detects and recognizes the parasites when they mature in the blood cells. As a way to protect the body, immune cells are released to attack and kill the parasites. However, through the years, the parasites have evolved in many ways to escape the attack of immune cells, including burying themselves in tiny blood vessels and producing sticky molecules on infected red blood cells.
The researchers also noted that malaria-infected red blood cells protect themselves from the immune system by attaching directly to non-infected red blood cells to form a flower-shaped structure known as a rosette.
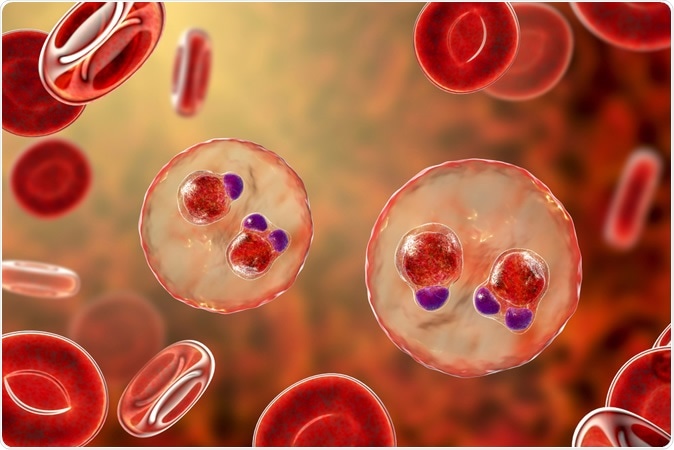
Malaria-infected red blood cells. 3D illustration showing ring-form trophozoites of malaria parasite Plasmodium falciparum inside red blood cells, the causative agent of tropical malaria. Image Credit: Kateryna Kon / Shutterstock
What is the rosette phenomenon?
The rosette phenomenon has been seen in all human malaria parasites and has been tied to disease severity though the exact function of the progression of malaria remains unknown.
Malaria, which is caused by the parasite Plasmodium falciparum, induce morphologic functional and antigenic changes in host red blood cell membranes. Recently, resetting has been important in understanding the pathogenesis of severe malaria, including cerebral malaria.

Plasmodium falciparum 3d illustration. Image Credit: Sciencepics/ Shutterstock
Previous work shows that the rosette phenomenon might work as a protection for the red blood cell infected with malaria. This helps the parasite prevent its clearance by the immune system.
Defense mechanism in malaria
To arrive at their findings and answer whether rosette helps the infected red blood cells evade the immune system, the team incubated phagocytes, a type of immune cells that protect the body by ingesting harmful foreign particles such as bacteria, dead cells, viruses, and parasites, with clinical samples of blood cells infected by malaria. This way, they can study the extent of rosette formation, and discovered that the resetting rate boosted by about 10 to 40 percent when there are phagocytes. The results suggest that the presence of immune cells stimulated the formation of rosettes by malaria-infected cells.
Further, the team wanted to see how the immune cells trigger rosette formation. To do this, they extracted various components of the blood and studied which ones were needed to form rosettes. The researchers discovered a substance known as human insulin growth factor binding protein 7 (IGFBP7), which is essential in rosette formation. Interestingly, when the researchers added the substance to two different malaria parasites, even if there aren’t any immune cells, it still triggered rosette formation.
Further, the team studied if the formation of rosette stimulated by the IGFBP7 could prevent the malaria-infected cells from being swallowed up and killed by phagocytes, in a process known as phagocytosis. They found that there was an increase in rosette formation when there was IGFBP7, but the number of infected RBCs that were eaten by the immune cells decreased.
The study can help pave the way for the development of new antimalarial drugs, which can lighten the burden of the disease, especially in tropical countries where the disease is taking lives.
Malaria is potentially fatal, with an estimated 228 million cases and 405,000 deaths in 2018. The most vulnerable are children who are five years old and below. The most affected region is Africa, which is home to 93 percent of all malaria cases, and 94 percent of all malaria deaths in 2018.
Journal reference:
Plasmodium-infected erythrocytes induce secretion of IGFBP7 to form type II rosettes and escape phagocytosis, Wenn-Chyau Lee, Bruce Russell, Radoslaw Mikolaj Sobota, Khairunnisa Ghaffar, Shanshan W Howland, Zi Xin Wong, Alexander G Maier, Dominique Dorin-Semblat, Subhra Biswas, eLife 2020;9:e51546 DOI: 10.7554/eLife.51546, https://elifesciences.org/articles/51546