Healthy lung cells support the survival of breast cancer cells, allowing them to hibernate in the lung before forming secondary tumors, according to new research from the Crick. The findings could help the development of new treatments that interfere with this behavior, reducing the number of secondary cancers.
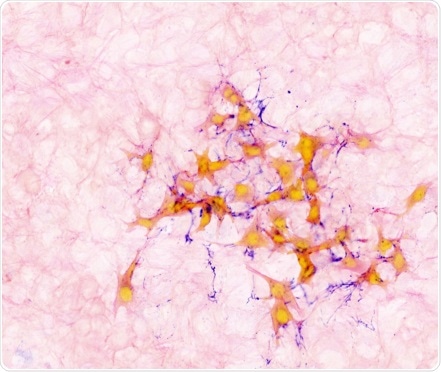
Image showing mouse breast cancer cells (orange) within lung tissue (light pink), connected with protein fibres (purple).
The study, published in Nature Cell Biology, used a mouse model to show that, after cancer cells from a breast tumor arrive in the lungs, a signal sent out from the lung cells causes cancer cells to change shape and grow protrusions that latch onto the lung tissue. The lung cells then protect them within the lung tissue.
By using a treatment that interferes with the growth of these protrusions on the breast cancer cells, the researchers found that mice who received the treatment grew fewer secondary tumors than the control mice.
The researchers then analyzed the genes that are turned on in the hibernating cells. This enabled them to find a key gene, sFRP2, that regulates the formation of cell protrusions and the survival of breast cancer cells in the lung.
Cancer can survive, hibernating in different parts of the body, for many years. By showing how the microenvironment around the cancer cell can support its survival, in our case how the lung cells help the breast cancer cells, opens the door to potential new treatments which target this relationship.”
Erik Sahai, co-lead author and group leader of the Crick’s Tumour Cell Biology Laboratory
The cancer cells were tested over the course of up to four weeks, during which they remained inactive. In comparison, other cell types continued to remain active, showing that the hibernation of these cells is due to a special relationship they have with the lung environment around them.
“The mechanism behind how cancer cells survive in tissues they have traveled to is not yet well understood. But with many cancers spreading around the body and consequently many patients suffering from relapses, a deeper understanding of the process is vital and something we’ll continue to explore,” says Marco Montagner, co-lead author and former postdoc in the Crick’s Tumour Cell Biology Laboratory, who is now based at the University of Padua.
Around 55,000 people in the UK are diagnosed with breast cancer each year. This cancer can spread through the blood or lymphatic system to another part of the body, commonly the lungs, liver, brain or bones. Where breast cancer spreads to the lungs, there can be a long time between the cells arriving in the lungs and the formation of a secondary tumor. This gap is one factor that explains why people may relapse a long time after the initial disease.
The researchers are continuing to explore the relationship between cancer and non-cancerous cells in a secondary location in the body. At the Crick, researchers are now studying what happens when cells from colorectal cancer and melanomas form secondary tumors in the liver. While at the University of Padua, studies are ongoing into the genes which are over-expressed in hibernating breast cancer cells.
Source:
Journal reference:
Montagner, M., et al. (2020) Crosstalk with lung epithelial cells regulates Sfrp2-mediated latency in breast cancer dissemination. Nature Cell Biology. doi.org/10.1038/s41556-020-0474-3.