Why is one small virus causing so much panic in the world today? The SARS-CoV-2 virus (short for severe acute respiratory syndrome coronavirus 2) that causes COVID-19 disease is spreading like wildfire, through over 200 countries and territories so far. Each new case means the virus has successfully been transmitted from one infected person to someone who was not previously infected.
Viruses are tiny bundles of DNA or RNA which have the ability to infect host cells, hijack the machinery of the host cell and then replicate. Once the host cell’s resources are exhausted, the viral particles are released to infect other cells. In this way, the viruses ensure their survival, often at the expense of the host.
The SARS-CoV-2 belongs to the same family as earlier coronavirus pathogens, the SARS CoV, and the MERS CoV, which caused several outbreaks of respiratory illness in 2002-03 and 2012. These were thought to have originated from bats but jumped the species barrier to infect humans. While SARS affected about 8,400 people with about 900 deaths, with a mortality rate of 9%, MERS hit about 2,500 people and killed about 850 of them, for a shocking fatality rate of 34%.
The coronavirus disease-2019 (COVID-19) has so infected over 900,000 victims so far, with the total number of deaths fast approaching 50,000 globally. But how does it spread?
.jpg)
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of a VERO E6 cell (blue) heavily infected with SARS-COV-2 virus particles (orange), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Scientists think the primary route of spread is from person to person through respiratory droplets. These are droplets of respiratory secretions containing viral particles that burst into the air with a sneeze or cough. If these come into contact with the moist mucous membranes covering the surfaces of the nose, eyes, or mouth, the viral particles can infect the epithelial cells and travel straight to the lungs and throat. The skin and hair are, in contrast, not as easily affected.
On the other hand, if the droplets fall on any surface and if uninfected people then touch that surface before the virus is inactivated, the hand is contaminated. If such people don’t wash their hands thoroughly immediately thereafter and touch the face, eyes, nose, or mouth, either their own or someone else’s, the same kind of transmission could occur, leading to infection.
Thirdly, infected people could get the droplets on their hands when they sneeze or cough, and then carelessly touch some other surface and contaminate it by not washing their hands immediately. Kissing or sharing straws, cups, lipsticks, or water bottles can all be potential sources of viral spread because all these items go into the mouth and can be contaminated by the virus if one of the persons sharing the item is infected with the virus.
Can COVID-19 spread through the air?
The most significant route of spread so far is through respiratory droplets, which can travel several feet. Studies seem to show that these droplets do not typically linger in the air but drop to the ground or the nearest flat surface in about 10 minutes. The good thing about this is that it shows that if a positive individual is in a room for a while, and then leaves, almost immediately, the air will be clear of the virus and safe for anyone to breathe.
How easily does the COVID-19 virus spread?
The problem with the SARS-CoV-2 is the high viral shedding by asymptomatic patients or people who have just begun to feel sick. In fact, several recent studies show that some infected people have no symptoms at all. At the same time, they shed the virus liberally, more like influenza than like SARS, where patients only shed the virus being tested when they were obviously sick.
A study from Germany came up with two interesting observations: not only was the virus replicating in the nose and throat, but infectious transmission ceased after an average of 10 days. Mildly symptomatic people became non-infectious in a week or so. However, the real surprise was that symptoms resembling a cold were just as commonly encountered as the classic fever and dry cough more characteristically described in Chinese studies.
From the time when the virus was known to be spreading within Wuhan, mathematical, and statistical modeling of the number of infections occurring internationally was used to predict disease trends in the broader population. Based on such trends, scientists like Qianying Lin say that every infected person could infect 2 to 3 other people. This is called the basic reproduction number, R0, and is an important criterion to gauge infectious diseases.
Lin says, “Unlike other studies that estimated the number as high as five to six, we have a modest estimation because we took the reporting ratio (the fraction of illness cases that were actually reported) – which was low at the early stage – into account.” The work was taxing, given the potential of the results to produce public panic. Yet, the team has continued to estimate the predicted spread accounting for newer factors such as self-isolation, quarantines, and lockdowns.
The newest study from Lin forecasts that if governments continue to crack down on unrestricted and non-essential movement harshly, the Wuhan outbreak could be brought down to zero by the end of April – not just for a day but permanently.
Other scientists push this number still higher, at 2 to more than three people, up to 11 in some estimates. This means that the SARS-CoV-2 virus isn’t like the SARS virus at all in terms of the ease of spread. And the rapid spread from asymptomatic people means it could be hard to stop the outbreak. Only time and further testing will tell.
Why does the COVID-19 virus spread so easily?
The SARS-CoV-2 virus has already infected more than one hundred times the number who were affected by SARS back in 2002. The reasons lie in its spike protein, which is responsible for binding to the host cell membrane. This S protein, as it is called, is distinctive compared to those of closely-related coronaviruses. It has an activation site that responds to a host cell enzyme called furin – which happens to be abundant in the lungs, liver, and small intestine, among other human tissues.
In other words, the virus can launch its attack on multiple organs. The presence of this site also makes it more efficient at spreading between human hosts, as is inferred by its presence in other easily spreading viruses like some influenza strains that cause severe illness. Only, these other viruses have this site on a hemagglutinin protein rather than on the S protein.
All experts don’t agree with this hypothesis. Among other factors, there is a significant difference between the two proteins; also, the flu virus responsible for the 1918 ‘Spanish flu’ pandemic doesn’t have a furin activation site at all. Virologist Peter White thinks such theories need to be tested in laboratory cell or animal experiments, because of the “unpredictable” nature of coronaviruses.
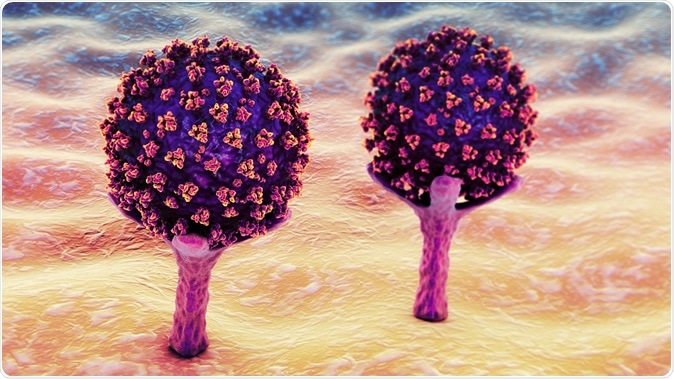
SARS-CoV-2 viruses are binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection. Conceptual 3D illustration credit: Kateryna Kon / Shutterstock
Another possibility is the high-affinity binding of the spike protein to the ACE2 receptor on human cells, ten times that of the corresponding protein in the SARS virus.