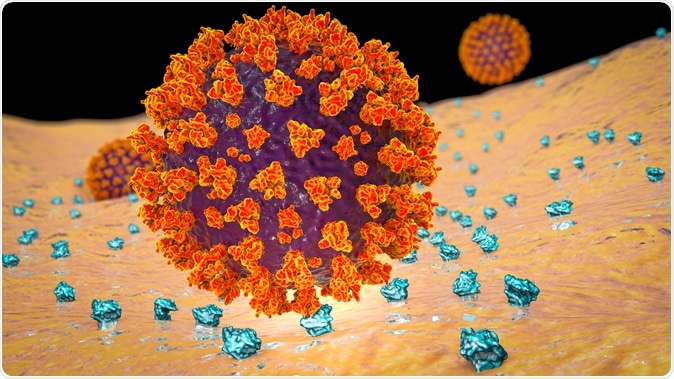
SARS-CoV-2 virus binding to ACE2 receptors on a human cell, the initial stage of COVID-19 infection, 3D illustration credit: Kateryna Kon / Shutterstock
The coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) early this year. Its symptoms range from none through mild to critically severe, leading to death in a few. Most severe cases have been reported in people over the age of 55 years with underlying medical illnesses such as COPD. The current study was motivated by the desire to identify increased levels of ACE2 in the bronchial epithelium of the lungs.
The study not only confirms earlier findings but shows, for the first time, that former smokers have lower levels of ACE2 than current smokers.
Researcher Janice Leung says, "The data emerging from China suggested that patients with COPD were at higher risk of having worse outcomes from COVID-19. We hypothesized that this could be because the levels of ACE-2 in their airways might be increased compared to people without COPD, which could possibly make it easier for the virus to infect the airway."
ACE-2 is an enzyme similar in function to angiotensin-converting enzyme (ACE), but different in that it not only (like ACE) converts angiotensin I to angiotensin II, which is a potent vasoconstrictor, but also further degrades angiotensin II to angiotensin (1-9) and angiotensin (1-7). These are potent vasodilators and could even be inhibitors of the vasoconstrictor renin-angiotensin system. ACE-2 is present in upper respiratory mucosa, lung mucosa, heart muscle, and gut lining. It seems to be an important molecule in the regulation of cardiovascular function.
How was the study done?
The researcher looked at samples from the lungs of 21 patients with COPD, which refers to a condition in which the lungs are chronically overinflated, thus reducing the capacity of the lung to push out old or stale air and bring in fresh oxygenated air. This, in turn, causes chronic hypoxia as it progresses.
The samples from the diseased lungs were compared with those from 21 healthy lungs. All of them were analyzed for ACE2 concentrations. They adjusted the final readings based on other factors, such as whether the people were lifelong non-smokers, were currently smoking, or had smoked in the past.
What did the study find?
The analysis showed that COPD patients had higher ACE2 levels in the lung samples, and so did current (but not former) smokers. In patients with COPD, the gene expression levels rose in direct proportion to the severity of the lung condition.
To extend their findings, they also checked them against two other groups, also studying the same thing – comprising, in total, almost 250 people, some of whom had smoked, some who had never smoked, and some who were smoking. The same pattern of ACE2 concentration was observed. Both non-smokers and those who had quit had lower ACE2 levels.
The limitations of the study included the observational design, which made it impossible to decide if other interventions for respiratory distress, such as bronchodilators or corticosteroids, played a role in determining how the ACE-2 gene was expressed in the airways. Secondly, the precise attributable risk due to smoking and COPD in severe COVID-19 illness, among other factors, is not clear. The extent to which the virus gained access through the gut or upper airway was also not studied.
Why is the study important?
Commenting, Leung said that the history of COPD and current smoking were independent risk factors for higher ACE2 levels in the airways. This, in turn, increases the risk that these patients will have severe illness. Against this backdrop, the advice about social distancing should be strictly followed by all patients with COPD, as well as regular and thorough handwashing with soap, as well as sanitizer use when soap and water are not available, to prevent their catching the often lethal virus.
However, the levels of ACE2 in non-smokers were low – no surprises there – but also in former smokers who had quit. The researchers suggest that this could be a powerful motivation to quit smoking: "There has never been a better time to quit smoking to protect yourself from COVID-19."
The observational aspect of the study has impressed many infectious disease specialists. However, they point out, the study shows why some people develop more severe infections than others but fails to communicate the potential role of inducing alterations in the ACE2 levels in treating such patients. It also doesn't really tell us anything about whether it is worthwhile to do this, in terms of increased survival, in patients with COPD who also become ill with COVID-19. Nonetheless, it is important to stress the need to quit smoking and to rapidly screen such individuals both to prevent and to diagnose the presence of COVID-19 in this high-risk group.
Journal reference:
Leung, J. A., Yang, et al. (2020) ACE-2 Expression in the Small Airway Epithelia of Smokers and COPD Patients: Implications for COVID-19, European Respiratory Journal 2020; in press https://doi.org/10.1183/13993003.00688-2020