The coronavirus disease (COVID-19) continues to threaten millions of people across the globe, and lockdowns appear set to remain in place in many countries amid rising death tolls, as governments decide whether to extend restrictions aimed at reducing the spread of the virus. Now, a new study reveals that the novel coronavirus has mutated into at least 30 different genetic variants, affecting different parts of the world.
The team of researchers, spearheaded by Chinese scientists Professor Li Lanjuan and her colleagues at the Zhejiang University in China, has found within a small pool of patients many mutations not previously reported. These mutations include rare changes that scientists had never imagined could happen.
The novel coronavirus, now officially called the severe acute respiratory coronavirus 2 (SARS-CoV-2), is an RNA virus, just like the viruses that cause measles and flu. These viruses are more prone to changes and mutations compared to DNA viruses.
As the SARS-CoV-2 ripples across the globe, scientists worry that the virus will mutate into something deadlier and become a more significant threat to humanity.
Mutations and rapid spread
To arrive at their findings, the researchers analyzed the strains from the 11 randomly chosen COVID-19 patients from Hangzhou in China, where there had been 1,264 confirmed cases. They tested how the virus can effectively infect and kills the cells in the body. The team identified more than 30 different mutations of the virus, wherein 19 were never seen before.
Some of the mutations boosted the ability of the virus to spread, while others strengthened its ability to invade cells. The team found that the deadliest mutations were seen in the ones spreading in Europe and New York. On the other hand, weaker strains were seen in some parts of the United States, such as Washington State.
“Current genomic survey data suggest that single nucleotide variants (SNVs) are abundant. However, no mutation has been directly linked with functional changes in viral pathogenicity,” the researchers wrote on the paper.
The paper, which was published in the online journal MedRxiv, highlights how studying the mutations can help provide a basis for vaccine development. The tricky part is with more mutations happening. It will take some time before a vaccine can be developed.
This is the first study to provide an insight into how a mutation could impact the severity of the disease. For instance, the virus in New York is stronger and more aggressive, and it has the highest infection toll in the country.
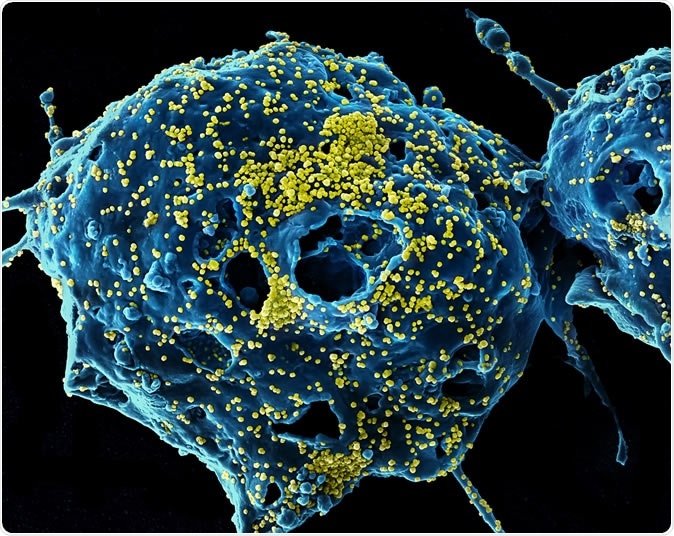
MERS Virus Particles Colorized scanning electron micrograph of Middle East Respiratory Syndrome virus particles (yellow) attached to the surface of an infected VERO E6 cell (blue). Image captured and color-enhanced at the NIAID Integrated Research Facility in Fort Detrick, Maryland. Credit: NIAID
However, the weaker mutation did not mean a lower risk for the population. Take, for example, two patients in the study in Zhejian, who are in their 30s and 50s, had contracted the weaker strain of the virus but became severely-ill. Though the patients had recovered, they required admission in the intensive care unit (ICU).
The team also revealed that some of the most aggressive strains of the coronavirus were able to generate 270 times the viral load of the weaker strains. Further, potent strains kill human cells fastest.
“Therefore, we provide direct evidence that the SARS-CoV-2 has acquired mutations capable of substantially changing its pathogenicity,” the team added.
The team believes the previous mutations that were not reported could be the reason behind the high death tolls in some parts of Europe and New York. The United States now has the highest number of confirmed cases and deaths, with 840,897 and 46,611, respectively.
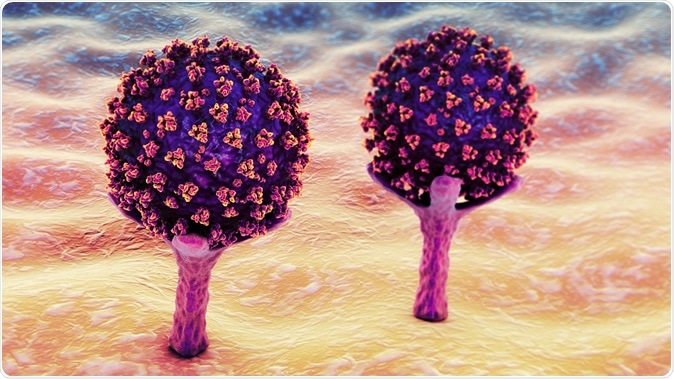
SARS-CoV-2 viruses are binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection. Conceptual 3D illustration credit: Kateryna Kon / Shutterstock
Effect of many mutation variants
With many mutations occurring in the virus, it may become more challenging to develop a vaccine that is effective in preventing the coronavirus disease. Patients with COVID-19 are being treated in hospitals using one treatment, regardless of the strain they have. The researchers suggest that knowing the different mutations can aid in providing the right treatment to patients. Also, they can determine actions to battle the virus.
Though the need for treatment or vaccine is urgent amid the coronavirus pandemic, it is essential to take into consideration the accumulating mutations.
Globally, the death rate topped 177,000, while the number of confirmed cases has reached a staggering 2.56 million people. The United States and some countries in Europe, such as Spain, France, Italy, Germany, the United Kingdom, and Turkey, have reported the highest number of cases.
Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source:
Journal reference:
- Yao, H., Lu, X., Chen, Q., Xu, K., Chen, Y., Cheng, L., Liu, F., Wu, Z., Wu, H., Jin, C., Zhengm M., Wu, N., Jiang, C., and Li, L. (2020). Patient-derived mutations impact the pathogenicity of SARS-CoV-2. MedRxiv. https://www.medrxiv.org/content/10.1101/2020.04.14.20060160v1