The current COVID-19 pandemic (caused by the severe acute respiratory syndrome coronavirus 2 or SARS-CoV-2) is our unprecedented reality, with approximately three million cases worldwide and more than 200 thousand deaths.
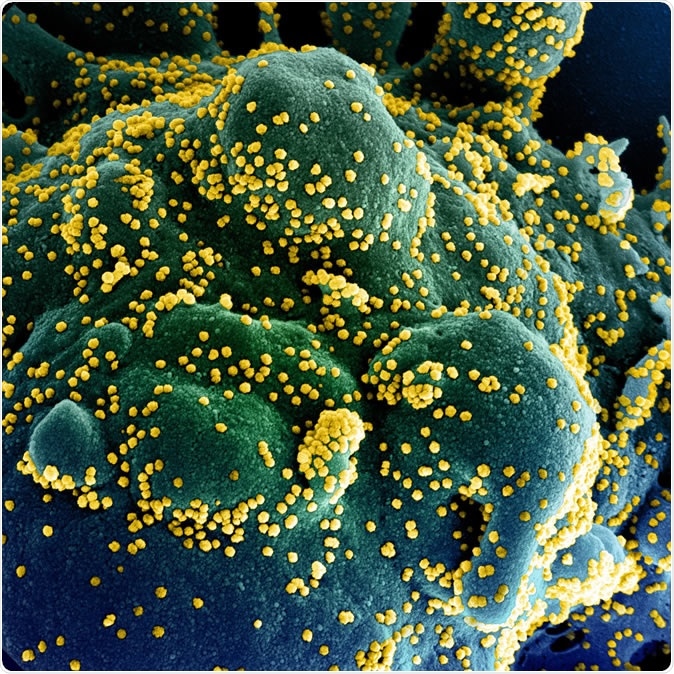
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (blue/green) heavily infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Severe types of COVID-19 disease are associated with increased levels of cytokines (such as interleukin 6, interleukin 10, and tumor necrosis factor-alpha); however, it is not clear whether this is an appropriate response or a dysregulated immune response known as 'cytokine storm'.
To untangle pathways that lead to either protective immunity or immune pathology, a momentous team effort by researchers from Stanford University School of Medicine and Stanford Immunology Program resulted in a publication available at medRxiv.
A complex methodological approach
Single-cell transcriptomics was utilized as the main approach to portraying the peripheral immune response in severe COVID-19 patients. For appraisal purposes, blood samples were collected from seven patients enrolled in the Stanford University ICU Biobank study, as well as six healthy controls.
The researchers used Seq-Well platform for single-cell RNA sequencing to separate cells of interest (most notably peripheral blood mononuclear cells) and perform initial steps of sample preparation. This is a low-cost, portable platform for sequencing cells at high throughput.
To address a plethora of challenges of RNA sequencing, the reads were aligned by using ultrafast universal STAR aligner, while count matrices were assembled with the use of dropEst pipeline. The latter is utilized for accurate molecular count estimation in such single-cell RNA sequencing experiments.
Gene pathway and upstream regulator analysis were accomplished with Ingenuity Pathway Analysis, which is a tool from QIAGEN for quick visualization and understanding of complex data (such as those yielded by this research endeavor).
Reduced function of the innate immune system
"Overall, we observed marked changes in immune cell composition and phenotype in SARS-CoV-2 infection compared to healthy controls, including depletion of innate immune cells such as NK cells and pDCs, and the induction of an interferon-stimulated gene (ISG) signature across multiple immune cell types", explain the researchers.
Plasmacytoid dendritic cells (pDCs) and natural killer (NK) cells are recruited as a form of innate antiviral response. Still, here the virus hampers this type of reaction and can, therefore, lead to more severe infection.
Furthermore, ISG signature can be a biomarker of beneficial immune response, but also, seemingly paradoxically, the induction of the specific subset of such signature may indicate an unfavorable response.
Correlates of immune dysregulation
In humans, Human leukocyte antigen (HLA) class II molecules are known to optimize the immune response against various viral agents by efficiently presenting viral antigens to T lymphocytes
Akin to some previous studies, the researchers here have found a decreased responsiveness to stimuli and downregulation of HLA class II in severe COVID-19 patients, resulting in poorer outcomes.
"As such, the marked downregulation of HLA class II molecules in COVID-19, particularly in severe disease with acute respiratory distress syndrome (ARDS), may reflect immune dysregulation that inhibits the generation of protective immunity", explain the researchers.
Moreover, peripheral lymphocytes and monocytes do not express significant amounts of pro-inflammatory cytokines, suggesting that circulating leukocytes are not significant contributors to potential COVID-19' cytokine storm'.
A closer look at the white blood cells
Albeit increased neutrophil counts have been reported in patients with severe forms of COVID-19 disease, the researchers from Stanford have not observed a significant increase of canonical neutrophil proportion within the tested samples.
"This suggests that the increase in neutrophils observed clinically may be due to the increase of this activated granulocyte subset," explain the authors. The exact role of granulocytes in the pathogenesis of COVID-19 represents a vital domain of future research.
In conclusion, this study is thus far a most comprehensive approach to develop a single-cell atlas depicting the peripheral immune response to severe COVID-19. The results may aid in informing novel treatment strategies, taking into account the mechanisms of immune dysregulation.
Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
Wilk, A.J. et al. (2020). A single-cell atlas of the peripheral immune response to severe COVID-19. medRxiv https://doi.org/10.1101/2020.04.17.20069930