SARS-CoV-2, which shows a 70% similarity in genetic sequence to the original SARS coronavirus (SARS-CoV) identified in 2003, is responsible for causing coronavirus disease (COVID-19) that predominantly affects the respiratory tract with potentially fatal consequences.
The scale of the current COVID-19 pandemic implies this virus may continue to circulate among humans, resulting in yearly seasonal outbreaks. After SARS-CoV and MERS-CoV, SARS-CoV-2 is the third highly pathogenic coronavirus which jumped to humans within the last 20 years – suggesting that zoonotic coronavirus spillovers may happen again in the future.
However, sparse information is available on coronavirus transmission and pathogenesis, as well as specific viral target organs. This is in part due to the lack of in vitro cell models that can accurately model host tissues.
Research group affiliated with the Erasmus Medical Center, University Medical Center Utrecht, Royal Netherlands Academy of Arts and Sciences, The Maastricht Multimodal Molecular Imaging Institute, Center for Molecular Medicine and Oncode Institute and Hartwig Medical Foundation aimed to appraise whether human gut enterocytes are also a viral target.
Can COVID-19 affect the intestines?
Even though the clinical presentation of COVID-19 is primarily linked to the respiratory system, gastrointestinal symptoms are also observed in a subset of patients. Moreover, viral genetic material (ribonucleic acid or RNA) can be found in rectal swabs, even after nasopharyngeal testing has yielded negative results – Implying gastrointestinal infection and a potential fecal-oral transmission route.
And indeed, the SARS-CoV-2 receptor angiotensin-converting enzyme 2 (ACE2) that confers viral entry is highly expressed on differentiated enterocytes, which are the most abundant epithelial cells in the human intestine (i.e., up to 80 percent of all epithelial cells).
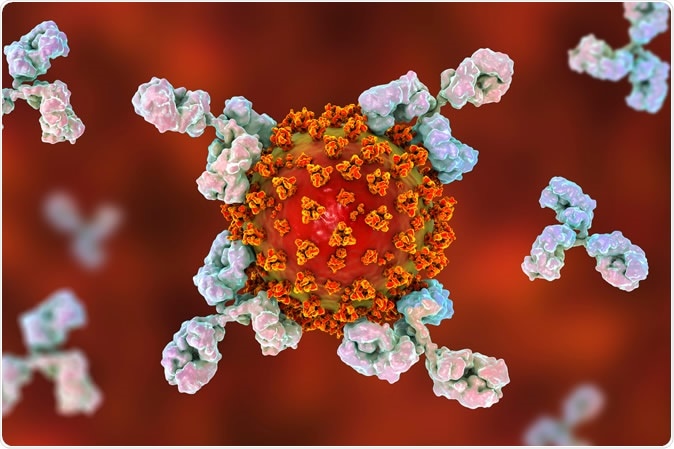
Antibodies attacking SARS-CoV-2 virus, the conceptual 3D illustration. Image Credit: Kateryna Kon / Shutterstock
This is why the research group from the Netherlands decided to use human small intestinal organoids to study infection patterns caused by SARS-CoV-2, but also by the original SARS-CoV. Intestinal organoids are basically 3D laboratory models of the human intestinal epithelium that allow patient-specific and robust in vitro appraisal of its properties after infection and/or inflammation.
Nucleic acids and viral particles inside cells
After demonstrating that both SARS-CoV and SARS-CoV-2 readily infect organoid-derived human airway epithelial cells, the researchers have also shown that they can productively infect human small intestinal organoids with the use of molecular techniques for detecting viral RNA.
Significant titers of infectious particles for both viruses were measured in all conditions; furthermore, in differentiated human small intestinal organoids, SARS-CoV-2 titers were stable even at 60 hours following the infection (on the other hand, SARS-CoV titers dropped significantly).
The infection of human small intestinal organoids was also demonstrated by confocal and transmission electron microscopy. Viral particles, ranging between 80 and 120 nanometers, were readily observed in the lumen of the organoid cells at the basolateral (facing adjacent cells in the underlying tissue) and apical side (facing the basement membrane) of enterocytes.
Human gut readily supports SARS-CoV-2 replication
Furthermore, the infection with SARS-CoV-2 induced a full signature of cytokines, and interferon-stimulated genes (ISGs) ascribed to type I and III interferon responses. These are known to confer antiviral defense on target cells and represent pivotal components of the innate immune response.
Their data also indicate that SARS-CoV-2 has the propensity to induce a more robust immune response than SARS-CoV in this type of laboratory model. And to successfully enter the cells, even low levels of ACE2 receptors may be sufficient, which means their infectious ability is better than previously thought.
"It appears of interest that we see at least equal infection rates of enterocyte-precursors and enterocytes whereas ACE2 expression increases ~1000-fold upon differentiation at the mRNA level", explains the study authors in their study available on the preprint server bioRxiv.
"Our data imply that human organoids represent faithful experimental models to study the biology of coronaviruses," study authors summarize their findings. "We conclude that intestinal epithelium supports SARS-CoV-2 replication", they add.
Gut epithelium definitely represents a rich model to study many different questions regarding SARS-CoV-2 pathogenesis and COVID-19 infection patterns. In the future, collaborative efforts on this type of basic research will be needed to inform further epidemiological measures.
Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.