COVID-19 is causing a pandemic situation in 187 countries and territories globally. Caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), it is massively impacting the health, survival, and economic well-being of millions around the world. A new study published on the preprint server bioRxiv* in April 2020 reports that low levels of specific immune cells, namely, CD8 T cells and NK cells, are linked to higher expression of the ACE2 molecule, which acts as a receptor for the CoV.
It is known that CoV has spike glycoproteins on the cell surface, which bind to molecules on the human host cell, called receptors. These receptors primarily include the angiotensin-converting enzyme 2 (ACE2), with other S-protein primers like TMPRSS2 working to facilitate the entry of the virus.
The SARS-CoV-2 virus has a 10 to 20-fold increased affinity for the human ACE2 receptor, and an increased concentration of these receptors makes it more vulnerable to these viruses.
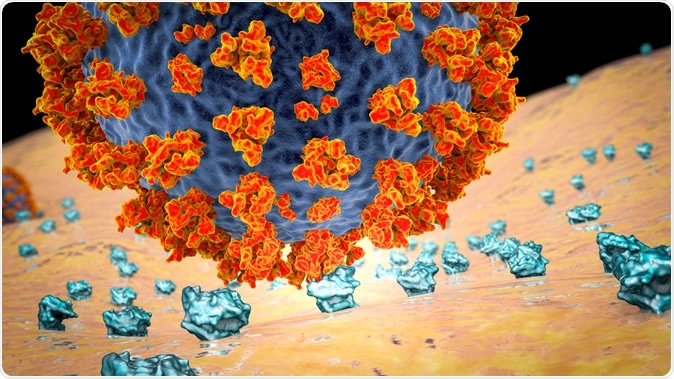
SARS-CoV-2 virus binding to ACE2 receptors on a human cell, the initial stage of COVID-19 infection. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Immune response of lung cells to viral infection
The virus targets the epithelial cells of the respiratory tract. These cells have pattern recognition receptors that help them recognize viral infection via the pathogen-associated molecular patterns (PAMPs). When these receptors are activated, a cascade of pro-inflammatory chemicals, particularly interferons (IFN) type I and type III, is triggered, activating the immune system.
In response, six types of white cells are recruited to the virally infected lung tissue. Dendritic cells sense infection and initiate an immune response. CD4 cells enhance cytokine production as well as facilitating a greater degree of contact between the CD8 T cells and dendritic cells. M1 macrophages also work together with the lung epithelium to combat the viral particles. Neutrophils phagocytose viral particles.
CD8 T cells and NK cells have cytotoxic activity, which helps to control viral infection early by eliminating the infected cells and preventing the spread of the viral particles to more healthy cells.
How was the study done?
The researchers aimed at uncovering the link between ACE2 expression and the expression of 7 types of white cells. They estimated the levels of CD8 T cells and NK cells, M1 macrophages, dendritic cells, CD4 cells, and neutrophils, in relation to the level of ACE2 in the lung cells, over 1,900 human lung tissue samples.
To test the association between phenotype and these observations, they included variables like sex, age, body mass, and race, and smoking status, in the analysis. They found that only four factors are useful in predicting ACE2 levels, namely, CD8 T cells, resting and activated NK cells, and M1 macrophages, and none of the phenotypic covariates.
SARS-CoV-2 is highly efficient at infecting its host, replicating and producing infectious particles in the human lung, compared to the SARS-CoV. The alveolar epithelial cells are a primary entry point for SARS-CoV-2, which expresses the ACE2 receptor.
However, it doesn’t induce inflammation via these pathways at first, in the infected human lung cells. Moreover, the occurrence of such inflammation is counterproductive, as IFNs directly increase the expression of the ACE2 receptor.
The lungs are the site of the most severe symptoms in severe infection. The occurrence of a ‘cytokine storm’ brings about acute respiratory syndrome (ARDS), with extensive lung damage, pneumonia, and progressive respiratory failure. As a result, the patient needs intensive care unit (ICU) admission and mechanical ventilation.
In other words, the targeting of the ACE2 receptor by IFNs means that virally induced rises in IFNs aimed at recruiting more immune cells also cause the ACE2 expression to rise, which could potentially worsen the infection.
The baseline levels of immune cells are, therefore, more important in preventing hyperactivation of the immune response in COVID-19 than in inducing immune reactions to other viruses.
What does the study show?
The study shows that there is a negative correlation between ACE2 expression and the levels of CD8 T cells, resting and activated NK cells, and M1 macrophages. The other white cells did not show this relationship.
Overall, most white cells that are involved in antiviral immunity are found at low levels in those lung tissues that have high ACE2 expression.
Both the number and functional status of the ‘early responder’ cytotoxic T cells are reduced significantly in the current infection. CD8 T cells in peripheral blood are reduced and functionally exhausted in patients with COVID-19, especially in older and sicker patients. Low CD8 T cells are associated with reduced survival.
NK cells are the first responders that recognize and clear virally-infected cells stimulated by cytokines or antibodies, or if the infected cells express induced-self ligands or viral antigens. However, in the early stages of COVID-19, the infected cells are ominously quiet concerning the induction of pro-inflammatory signals. Later on, the NK cell count drops, and the cells themselves show evidence of exhaustion.
Post-infection, the innate immune system needs to be activated rapidly to eliminate the infective agent, typically by the release of inflammatory chemicals from infected cells. However, this reaction is typically not seen in the infected lung tissue, which fails to stimulate the production of several important molecules that would attract other immune cells to the fight.
The study concludes, “The link that we identified between high baseline ACE2 expression and reduced cytotoxic lymphocyte levels in human lung tissue prior to SARS-CoV-2 infection is striking. This may predict the long-term outcome of individuals infected with COVID-19.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources