The COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has turned the world's attention to the immune system. However, our immune system can act as a double-edged sword in that it can severely damage our body while fighting the virus.
From a clinical standpoint, COVID-19 resembles a typical community-acquired severe respiratory infection that occurs approximately one week after nonspecific flu-like symptoms; however, it exhibits a broader range of severity than MERS and original SARS infections.
The reason for such pronounced heterogeneity in individual sensitivity to COVID-19, as well as the potential roles of age and comorbidities (beyond their association with clinical worsening), are inadequately understood.
As even individual cases in this early stage of the pandemic may shed some light on this pertinent issue, a group of researchers from France reported their findings after the admission of one patient to the Bichat–Claude Bernard Hospital ICU in January 2020.
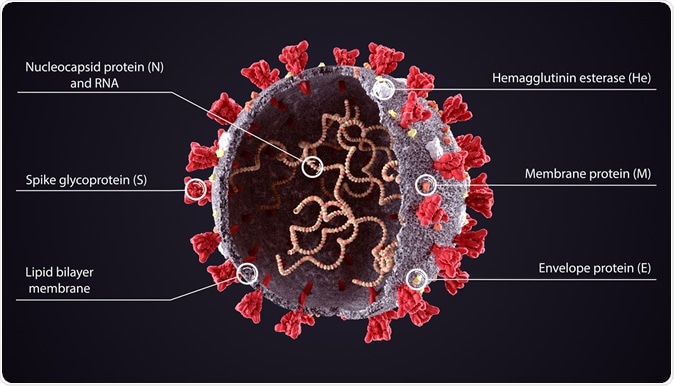
3D diagram of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) structure. Image Credit: Orpheus FX / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Meticulous case study
The article states that an 80-year-old man visited the emergency department due to unremitting fever, diarrhea, purulent sputum, and difficulties breathing. A medical examination suggested a lower respiratory tract infection, while routine blood tests revealed severe hypoxemia (low blood oxygen) and an elevated level of C-reactive protein (an inflammatory marker).
He was not immediately considered as a potential COVID-19 patient (since he did not fulfill the case definition), but appropriate precautions were taken anyway. Nonetheless, very quickly, he developed multiorgan failure with acute respiratory distress syndrome (ARDS), liver failure, acute kidney injury, and sepsis-like shock with a fatal outcome.
The presence of SARS-CoV-2 was subsequently confirmed by semi-quantitative reverse-transcriptase polymerase chain reaction (RT-PCR) on nasopharyngeal swabs, per the guidelines of the World Health Organization (WHO).
Other clinical, biological, and radiological data were accurately recorded from computerized medical records, and the researchers also collected information on the dates of disease onset, at-risk contact, and travel details.
Immune cell phenotyping was performed by flow cytometry, and a total of 72 analytes were quantified in heat-inactivated serum samples by multiplex magnetic bead assays or enzyme-linked immunosorbent assay. The hierarchical clustering of cytokines was also pursued.
Intense reaction of the immune system
The patient showed marked cell activation with the expansion of a specific subset of T cells. Both CD4+ and CD8+ T cells were dramatically higher when compared to control patients, as well as the production of proinflammatory cytokines (resulting in a 'cytokine storm').
Strikingly, the researchers observed a dramatically high level of Tγδ cells throughout the clinical course of his disease, which is a subset of immune cells crucial for antiviral immune responses, epithelial cell maintenance, and tissue recovery.
An expansion of antibody-secreting cells and exhausted memory B cells was also observed; however, the humoral response of this patient was not interrogated because a validated serological test was not available at that moment.
Another critical finding is persistent lymphopenia, which is habitually reported in several severe viral diseases. This case clearly showed how the aforementioned finding could be a predictive factor for increased 28-day mortality.
Consequently, performing a lymphocyte count early after admission is basically a simple blood test that could be utilized as a prognostic marker to explain early co-infections in severe viral diseases feasibly.
"It clearly shows that the immune alterations are dynamic," said study authors. "In the first phase, the innate immune system, driven by monocytes, macrophages, and Tγδ lymphocytes, is activated and leads to T-lymphocyte exhaustion," the team said.
The activation of B lymphocytes subsequently follows and contributes to a significant humoral response, and then finally, endothelial activation, cell cytotoxicity, and apoptosis are observed.
Balance is the key
The fine balance between viral factors and the host response (when the latter is exacerbated) appears to be pivotal for the clinical course and prognosis of the disease. Likewise, the intensity of the inflammatory response may play a substantial role in the pathogenesis of SARS-CoV2 – most notably in the airways.
"An in-depth longitudinal analysis of the immune profiles of our case showed dramatic alterations in the homeostasis of all blood cell populations, reflecting severe disturbances in innate and adaptive immunity," study authors explain their findings.
"It is difficult to correlate these features with clinical worsening from a single case, but a careful follow-up of these profiles in patients in ICUs may help to identify new prognostic markers or those of COVID-19 severity", they add.
Lessons learned
Overall, this case report underscores the need to combine two complementing approaches to hamper disease severity: using an antiviral to control viral replication and limit the source of hyper inflammation, and then using a specific immune modulator that targets the cytokine storm to potentiate this effect.
"The lack of knowledge of the pathophysiology of this new infection, the severity of the cases, and the absence of confirmed therapies have been critical challenges for all physicians and intensivists since the beginning of this year", emphasize study authors.
"In an epidemic context, it is crucial to rapidly improve our understanding of the disease to manage patients better and to share knowledge on the most severe cases and learn from them", they conclude.
In any case, the introduction of specific interventions should be further appraised in well-designed studies. In the meantime, this longitudinal analysis may help to determine the timing of such interventions and provide some recommendations for the clinical follow-up of life-endangered patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Bouadma, L. et al. (2020). Immune alterations during SARS-CoV-2-related acute respiratory distress syndrome. medRxiv. https://doi.org/10.1101/2020.05.01.20087239
- Peer reviewed and published scientific report.
Bouadma, L., Wiedemann, A., Patrier, J., Surénaud, M., Wicky, P.-H., Foucat, E., Diehl, J.-L., Hejblum, B. P., Sinnah, F., de Montmollin, E., Lacabaratz, C., Thiébaut, R., Timsit, J. F., & Lévy, Y. (2020). Immune Alterations in a Patient with SARS-CoV-2-Related Acute Respiratory Distress Syndrome. Journal of Clinical Immunology, 40(8), 1082–1092. https://doi.org/10.1007/s10875-020-00839-x. https://link.springer.com/article/10.1007/s10875-020-00839-x.