Researchers from Johns Hopkins University School of Medicine have found that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus could spread via ocular or eye surfaces. This is because the receptor where the virus binds – the ACE2, is also expressed on human eyes, they note. The study titled, “ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection,” was published online at the preprint server biorxiv prior to peer review.

ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Image Credit: photoJS / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What was the study about?
The researchers wrote that some patients with COVID-19 disease had shown signs and symptoms on their conjunctiva. Teardrop samples have also shown the SARS-CoV-2 virus. Researchers explained that eyes could be one of the entry points for the virus, and those who are infected may carry and transmit the virus in their eye secretions. The objective of this study was to “determine whether ocular surface cells possess the key factors required for cellular susceptibility to SARS-CoV-2 entry/infection,” wrote the receptors.
They explained, “The ocular surface could potentially serve as a portal of entry through exposure to aerosolized droplets or hand-eye contact.” The team of researchers was led by Lingli Zhou of the Department of Ophthalmology, Johns Hopkins University School of Medicine, Baltimore.
Wang Guangfa, a Peking University, respiratory disease specialist, had speculated that he had been infected with the virus during the initial phases of the COVID-19 pandemic because he was not wearing protective visors. At that time, China had recorded only 26 deaths due to the unknown acute respiratory distress syndrome. Wang complained of redness of eyes after his exposure and after a few days went on to develop characteristic pneumonia due to COVID-19.
The novel coronavirus or SARS CoV-2 was first discovered in December 2019 in Wuhan, Hubei province of China. It caused unknown cases of pneumonia and deaths. Since then, the infection has rapidly traversed the world, and on the 11th of March this year, it was declared a global pandemic by the World Health Organization (WHO). To date, it has infected over 4.1 million people across the globe and killed hundreds of thousands of people. Because of the novel nature of the virus, much remains to be explored regarding the infective process of the virus.
What was done?
For this study, the team looked at ten whole eye specimens from deceased persons and conjunctival specimens collected after surgery. The specimens were not from any person who had COVID-19. In these eyes, they looked for the ACE2 receptor. This receptor is the key factor that is responsible for binding with the virus and allows entry of the virus into the host cell. The presence of this receptor and the cell surface protease enzyme - TMPRSS2 can allow the entry of the virus into the eyes. The ACE2 receptor, they wrote, binds to the spike protein on the virus and allows the entry of the virus into the host cell.
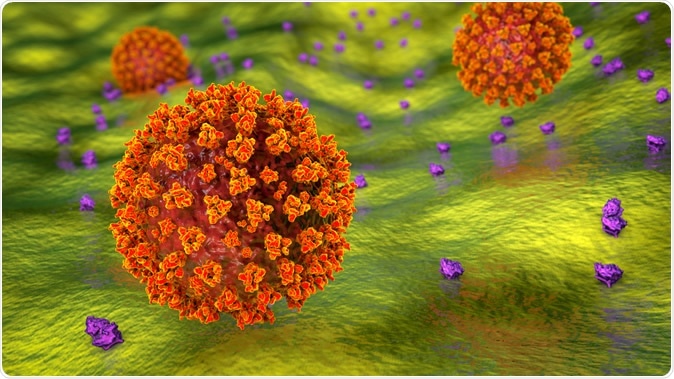
SARS-CoV-2 virus binding to ACE2 receptors on a human cell, the initial stage of COVID-19 infection. Illustration Credit: Kateryna Kon / Shutterstock
What was found?
The researchers found from all the specimens of eyes using immunohistochemical analysis that there was a distinct presence of the ACE2 receptor on the “conjunctiva, limbus, and cornea”. They noted that on the superficial conjunctiva and epithelial surfaces of the cornea, there was a prominent presence of the ACE2 receptors from the surgical specimens of the conjunctival epithelium on the superficial epithelium and the substantia propria. The eye and conjunctival specimens were also found to express the protein breaking enzyme or protease – TMPRSS2, which was also conducive to the spread of the virus through the eyes.
Next, the team conducted western blot analysis of the protein lysates found on the corneal epithelium from the refractive surgeries revealed expression of both ACE2 receptors and the protease TMPRSS2.
Authors wrote, “Together, these results indicate that ocular surface cells including conjunctiva are susceptible to infection by SARS-CoV-2, and could, therefore, serve as a portal of entry as well as a reservoir for person-to-person transmission of this virus.” They also wrote that conjunctivitis was seen in 30 percent of cases of COVID-19, and thus this theory held.
Conclusions and implications
The study shows that eye surfaces could be a portal of entry for the novel coronavirus. This could also serve as a “reservoir for person-to-person transmission” of the SARS-CoV-2. They called the conjunctival and corneal epithelial cells as a “secondary site of infection following respiratory tract” or even the “initial portal of entry to an individual.”
Health care workers need to wear goggles and face visors and masks to protect their eyes to explain researchers. Authors wrote that this study “highlights the importance of safety practices in the general community to prevent infection and spread (hygiene, face masks) and need for extra caution among ophthalmologists.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection, Lingli Zhou, Zhenhua Xu, Gianni M Castiglione, Uri S Soiberman, Charles G Eberhart, Elia J Duh, bioRxiv 2020.05.09.086165; doi: https://doi.org/10.1101/2020.05.09.086165
- Peer reviewed and published scientific report.
Zhou, Lingli, Zhenhua Xu, Gianni M. Castiglione, Uri S. Soiberman, Charles G. Eberhart, and Elia J. Duh. 2020. “ACE2 and TMPRSS2 Are Expressed on the Human Ocular Surface, Suggesting Susceptibility to SARS-CoV-2 Infection.” The Ocular Surface 18 (4): 537–44. https://doi.org/10.1016/j.jtos.2020.06.007. https://www.sciencedirect.com/science/article/pii/S154201242030104X.