The placentas had more features of maternal vascular malperfusion (MVM), a recognized pattern of damage to the placenta that is associated with adverse pregnancy outcomes.
Examples of these adverse outcomes have previously been demonstrated, including reduced fetal growth, pre-eclampsia, premature birth, and stillbirth.
Jeffery Goldstein and colleagues say the findings indicate that increased monitoring during pregnancy may be warranted in cases of coronavirus disease 2019 (COVID-19).
A pre-print version of the paper is available on the server medRxiv*, while the article undergoes peer review.
Interest in the effects of SARS-CoV-2 on pregnancy
People in the fields of obstetrics and pediatrics are currently keen to understand the effects that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and the associated COVID-19 may have on pregnant women and their babies.
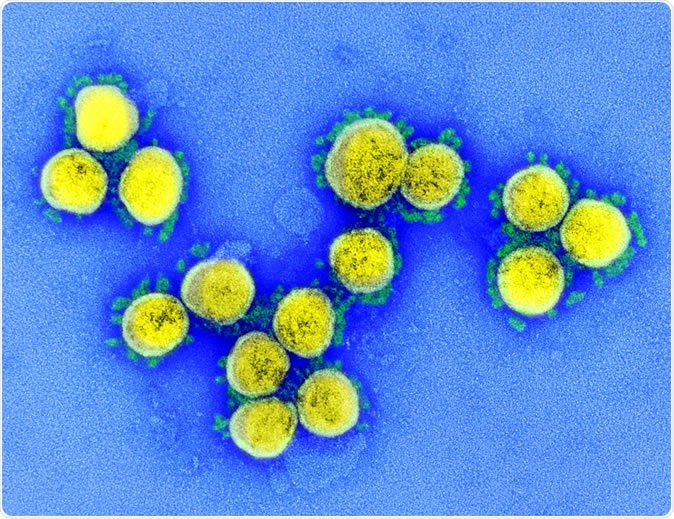
SARS-CoV-2 - Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The SARS-CoV epidemic that was identified in 2003 is thought to have affected about 100 pregnant women globally. Some studies showed that cases among pregnant women were associated with a severe infection in the mother and an increased risk of miscarriage and maternal death.
Studies have also suggested that the Middle East respiratory syndrome (MERS) is associated with adverse maternal and pregnancy outcomes.
Reports on COVID-19 infection among pregnant women are starting to emerge; one Chinese study reporting on placental findings described increased deposition of perivillous fibrin, multiple villous infarcts, and chorangioma.
However, “there is, to the best of our knowledge, no published case series in the English literature of placental pathology in women diagnosed with COVID-19 during pregnancy,” writes Goldstein and team.
Examining the placentas of pregnant women with COVID-19
Now, the researchers have examined the placentas of 16 women with COVID-19 who delivered between March 18th and May 5th, 2020.
They compared the findings with those from placental examinations of historical controls and those with a history of melanoma.
The researchers say one strength of their study is the inclusion of two distinct sets of controls. Placentas are only clinically examined in cases of an indication, such as disease or a birth complication.
“Melanoma history is an indication for placental examination but is considered independent of pregnancy outcome, and therefore some have advocated using these patients as a control,” explains the team.
Fourteen of the women had full-term births; one gave birth at 34 weeks, and one woman miscarried at 16 weeks. The latter case was not included in the statistical analysis, which was designed to assess third-trimester births only.
What did the researchers find?
The researchers say that despite the small size of the study population, some trends were observed.
“Compared to controls, third trimester placentas were significantly more likely to show at least one feature of maternal vascular malperfusion (MVM),” writes the team.
Twelve of the 15 women with COVID-19 had features of MVM, compared with 7,754 of 17,479 controls overall and 59 of 215 controls with a history of melanoma.
Examples of these MVM features included intervillous thrombi and chorangiosis.
In reference to the significant relative increase in intervillous thrombi among COVID-19 cases, the authors say: “In the context of research suggesting an increase of thrombotic and thromboembolic disorders in COVID-19, these may represent placental formation or deposition of thrombi in response to the virus.”
The authors say the fact that chorangiosis was significantly more common among COVID-19 cases is also interesting since it is associated with reduced oxygen saturation and is often observed in women who live at high altitudes.
However, “while the association between a respiratory virus and a finding sometimes seen in maternal hypoxia is interesting, the small sample size and confounding factors make it difficult to draw any conclusions at this time,” they add.
The study also found there was no increase in rates of acute inflammation pathology (AIP) and chronic inflammation pathology (CIP) among COVID-19 cases. The authors say this is relevant, given that SARS-CoV-2 is a virus and would be expected to trigger inflammation.
“Indeed, both categories of disease were less prevalent in COVID-19 patients, AIP significantly so,” the researchers write.
All infants born to mothers with COVID-19 tested negative for SARS-CoV-2
Throat swabs taken from infants born to mothers with COVID-19 showed that all were negative for SARS-CoV-2.
“This corroborates existing evidence that vertical transmission of the virus is uncommon, and suggests that placental changes if caused by COVID-19, are related to maternal infection and inflammation rather than fetal infection,” says the team. “In determining which placental anomalies are attributable to SARS-CoV-2 infection, we would argue that statistically significant associations identified in controlled studies, such as this one, are the appropriate first step."
The authors say their findings suggest an association between COVID-19 infection during pregnancy and abnormal maternal circulation, as well as providing insights into previously observed associations between adverse pregnancy outcomes and the infection.
“Collectively, these findings suggest that increased antenatal surveillance for women diagnosed with SARS-CoV-2 may be warranted,” they conclude.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Placental pathology in COVID-19 Elisheva D Shanes, Leena B Mithal, Sebastian Otero, Hooman A Azad, Emily S Miller, Jeffery A Goldstein medRxiv 2020.05.08.20093229; doi: https://doi.org/10.1101/2020.05.08.20093229
- Peer reviewed and published scientific report.
Shanes, Elisheva D, Leena B Mithal, Sebastian Otero, Hooman A Azad, Emily S Miller, and Jeffery A Goldstein. 2020. “Placental Pathology in COVID-19.” American Journal of Clinical Pathology 154 (1): 23–32. https://doi.org/10.1093/ajcp/aqaa089. https://academic.oup.com/ajcp/article/154/1/23/5842018.