Among patients admitted to hospital with coronavirus disease 2019 (COVID-19), testing positive for immunoglobulin G (IgG) antibodies against SARS-CoV-2 was associated with lower viral loads and a potentially lower risk of mortality.
The findings indicate that levels of anti-SARS-CoV-2 IgG antibodies could serve as a biomarker of disease course and the risk of infected individuals transmitting the virus to other people.
Among patients who tested positive for the antibodies (referred to as seroconversion), a high viral load was rare.
In addition, individuals who had a higher viral load on admission to hospital were at a more than 4-fold greater risk of death within 30 days (30-day mortality).
“Our data provide support for a disease model in which the development of anti-SARS-CoV-2 immune response leads to control of the virus in humans,” says the researchers. The data also “provides further support for quantitative viral load assessment, especially on hospital admission,” they add.
A pre-print version of the paper can be accessed in bioRxiv* while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Accurate tests are increasingly becoming available
The COVID-19 pandemic that has rapidly spread across the globe since its outbreak in Wuhan, China last year, is associated with high rates of morbidity and mortality.
According to Alexander Greninger and colleagues, since concerns first emerged over features of SARS-CoV-2 testing, accurate tests are increasingly becoming available.
For example, an anti-SARS-CoV-2 nucleocapsid IgG assay the team recently tested proved to be sensitive and specific in the detection of previous infection.
However, there is a lack of reliable data on virologic features and clinical outcomes to support these results, say the researchers.
Now, the team has assessed these features associated with seropositivity and seroconversion to SARS-CoV-2 among patients admitted to hospital with COVID-19.
The researchers identified 245 patients who had reverse transcription-polymerase chain reaction (RT-PCR) results that were positive for SARS-CoV-2 and tested their blood for IgG antibodies.
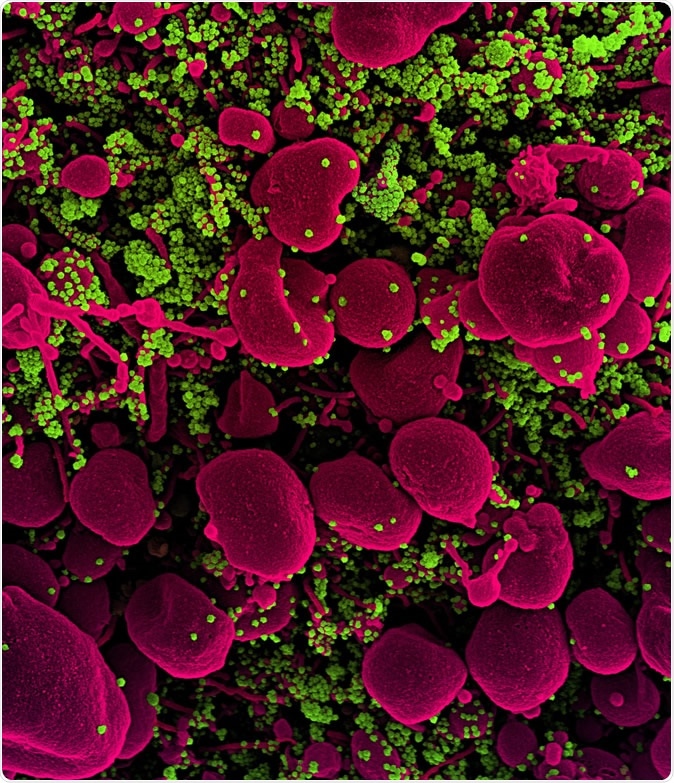
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (pink) heavily infected with SARS-COV-2 virus particles (green), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
What did the researchers find?
Analysis of quantitative RT-PCR and serology data revealed that only one individual who had anti-SARS-CoV-2 IgGs also tested positive for SARS-CoV-2 infection.
The team reports that the IgG level was inversely correlated with SARS-CoV-2 viral load.
To further test the association, the team assessed patients with more than three measures of anti-SARS-CoV-2 IgG and viral load. This showed that along with a decreasing viral load in association with increasing IgG, biomarkers of inflammation also decreased, while lymphocyte counts increased.
To test whether there was an association between seroconversion or high viral load and mortality, the team assessed SARS-CoV-2 viral load among 109 individuals and anti-SARS-CoV-2 IgG levels among 114 individuals on hospital admission and 30-day all-cause mortality since the day patients tested positive for infection.
After adjustment for serostatus of SARS-CoV-2, age, and gender, the viral load on hospital admission was significantly associated with all-cause 30-day mortality.
Patients with a higher viral load were at a 4.2-fold increased risk for mortality compared with patients who had a lower viral load.
Thirty-three percent (38) of the 114 patients tested for IgG had seroconverted before they were admitted to hospital, and this seroconversion was associated with a trend towards lower mortality. However, it did not reach statistical significance.
Greninger and colleagues say the association may not have reached significance due to the limited size of the study population.
“Antibodies are indicative of a protective anti-viral response”
“While our data do not directly assess the potential for ongoing immunity against future infections of SARS-CoV-2, they indicate that high viral loads rarely coexist with SARS-CoV-2 seropositivity and that antibodies are indicative of a protective anti-viral response and reduced 30-day all-cause mortality,” say the researchers.
“The association of the presence of anti-SARS-CoV-2 nucleocapsid IgG with lower viral load indicates antibodies may serve as a biomarker for COVID-19 disease course and infectious risk of the individual to the community,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Greninger A, et al. Anti-SARS-CoV-2 IgG antibodies are associated with reduced viral load. bioRxiv 2020. doi: https://doi.org/10.1101/2020.05.22.20110551
- Peer reviewed and published scientific report.
Bryan, Andrew, Susan L Fink, Meghan A Gattuso, Gregory Pepper, Anu Chaudhary, Mark H Wener, Chihiro Morishima, Keith R Jerome, Patrick C Mathias, and Alexander L Greninger. 2020. “SARS-CoV-2 Viral Load on Admission Is Associated with 30-Day Mortality.” Open Forum Infectious Diseases 7 (12). https://doi.org/10.1093/ofid/ofaa535. https://academic.oup.com/ofid/article/7/12/ofaa535/5952472.