The novel coronavirus, which first emerged in December 2019 in Wuhan City, China, has spread across the world, with more than 6.37 million people infected. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affects the respiratory tract and may cause potentially fatal pneumonia.
Now, in a significant scientific study, a team of researchers at the University of North Carolina Health Care (UNC) have mapped how SARS-CoV-2, the virus that causes the coronavirus disease (COVID-19), infects the nasal cavity, the airways, and down to the lungs.
Dominant site of infection
The coronavirus significantly infects the nasal cavity, where it replicates specific cell types. It then infects and replicates progressively less well in the cells in the lower respiratory tract, including the lungs. The team notes that the dominant initial site of replication and infection is the nasal cavity.
The study published in the journal Cell, suggests that the virus becomes established in the nasal cavity first, before being aspirated to the lungs where it causes severe symptoms of pneumonia, including the difficulty of breathing. The team notes that the later stage of infection only occurs in some cases, with some people experiencing no symptoms, while others may need hospital care.
“If the nose is the dominant initial site from which lung infections are seeded, then the widespread use of masks to protect the nasal passages, as well as any therapeutic strategies that reduce the virus in the nose, such as nasal irrigation or antiviral nasal sprays, could be beneficial,” Dr. Richard Boucher, the James C. Moeser Eminent Distinguished Professor of Medicine and Director of the Marsico Lung Institute at the UNC School of Medicine, said.
Mapping the infection
The research team aimed to understand which cells in the airway get infected by SARS-CoV-2 and how it travels to the lungs, particularly in patients who develop pneumonia. Severe COVID-19 disease typically affects those who are high-risk, including older adults, those who are immunocompromised, and those with underlying health conditions, including lung disease, heart disease, hypertension, and diabetes.
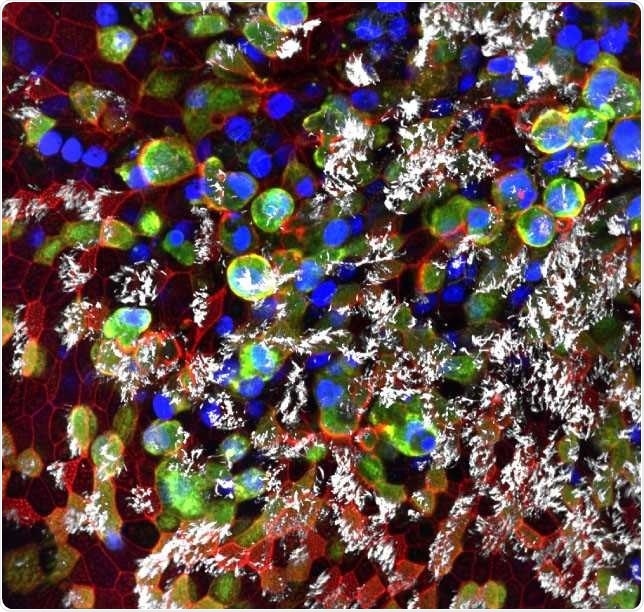
SARS-CoV-2 infected epithelial cells collected from healthy human bronchi. (Teresa Mascenik, the Randell Lab, UNC SOM)
To arrive at their findings, the researchers used various isolates of SARS-CoV-2 to determine how efficiently they could infect cultured cells taken from the different parts of the airways, including the nasal cavity, throat, airways, and the lungs.
The team has found a prominent pattern of continuous gradient or variation. The cells in the nasal cavity demonstrate high infectivity of SARS-CoV-2 in its cell linings, while the cells lining the throat and bronchi had less infectivity. The lowest infectivity was seen in lung cells.
Further, they also found that there are more angiotensin-converting enzyme 2 (ACE2s), the cell surface receptor where the virus binds to infect cells, on the cells lining the nasal cavity than on the surface of lower airway cells. This may explain why the cell lining in the upper airway is more vulnerable to infection.
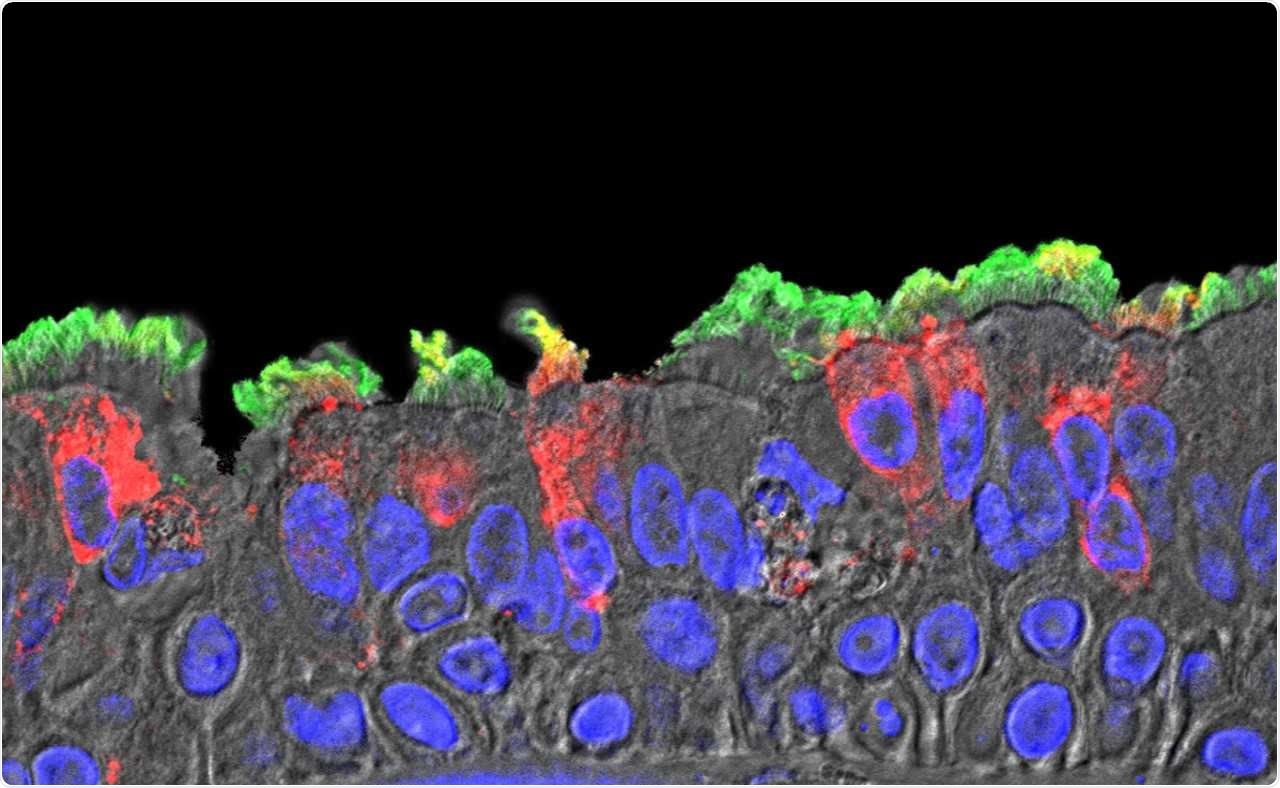
SARS-CoV-2 (red) infected ciliated cells in the COVID-19 patient's bronchi. (Takanori Asakura, PhD, the Boucher Lab, UNC SOM)
The course of infection
The team conducted further experiments on two protein-cleaving enzymes, called furin and TMPRSS2. These enzymes, which are found on human cells, are used by SARS-CoV-2 to re-shape essential virus proteins and enter the human cells for infection. The team also revealed that when there are elevated levels of these enzymes, the virus has an increased ability to infect cells and replicate.
They found that SARS-CoV-2 can infect airway-lining cells, known as epithelial cells, to a limited extent. However, the team discovered that the virus does not infect other airway cells. The virus did not infect club cells, even if these cells express both ACE2 and TMPRSS2. Also, the same types of airway epithelial cells from various human donors vary markedly in their vulnerability to infection.
The team notes that the findings highlight that there are still undiscovered factors in airway cells that can help determine the course of infection in people. This sheds light on the reason why some people may be asymptomatic, and others may experience more severe consequences, such as respiratory failure and death.
The researchers mapped the sites of infection in the lung of patients who had died from COVID-19. They unveiled that the sites of infections demonstrated patchiness and other characteristics showing that the infection occurs higher in the airway.
“These findings highlight the nasal susceptibility to SARS-CoV-2 with likely subsequent aspiration-mediated virus seeding to the lung in SARS-CoV-2 pathogenesis. These reagents provide a foundation for investigations into virus-host interactions in protective immunity, host susceptibility, and virus pathogenesis,” the researchers wrote in the paper.
The study results can pave the way for future studies on SARS-CoV-2 that may help develop therapeutics and strategies to reduce transmission and severity of COVID-19. Also, the study underscores the importance of wearing masks to limit the spread of the virus.
Source:
Journal reference:
- Hou, Y., Okuda, K., Edwards, C., Randell, S., Boucher, R., Baric, R. et al. (2020). SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell. https://www.cell.com/cell/fulltext/S0092-8674(20)30675-9