A new study has shown that anticardiolipin antibodies are associated with the novel coronavirus infection or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19. The study titled, “Clinically significant anticardiolipin antibodies associated with COVID-19,” was essentially two case reports from the researchers at the Department of Pulmonary and Critical Care Medicine and the Department of Medicine, Staten Island University Hospital, Staten Island, NY. The research is published in the latest issue of the Journal of Critical Care.
The COVID-19 pandemic to date has affected over 7.35 million persons across the world and killed over 416,000. The virus SARS-CoV-2 spreads rapidly from person to person, and there are challenges presented to the healthcare system owning to its infectivity and unpredictable course of action.
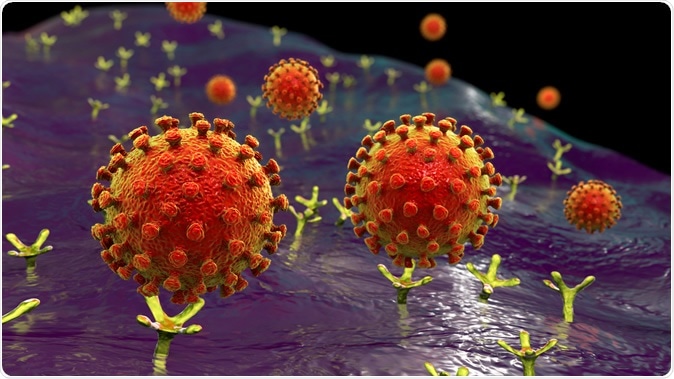
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection, conceptual 3D illustration credit: Kateryna Kon / Shutterstock
The team writes that there is a distinct possibility of coagulopathy or increased blood coagulation among those who are critically ill. Venous and arterial thrombotic events have been reported. They cite previous studies, for example, one from the Netherlands that shows that these thrombotic events leading to increased coagulation are seen in around 31 percent of patients testing positive for COVID-19.
This report was a detailed account of two cases that required critical care in New York City in April 2020. The researchers speculate the case behind such hyper-coagulability or thrombotic events, which could include prolonged immobilization, lowered blood oxygen or hypoxia, and “disseminated coagulopathy.” They also found that anticardiolipin antibodies were raised among both the cases and could be a key factor determining the course of the disease.
Case 1
This was a case of a 29-year-old female who presented to the emergency with vomiting and abdominal pain. She had a history of hemoglobin S-C disease, the authors of the study wrote. In addition, she had fever, cough, and generalized body ache. She was found to be positive for the SARS-CoV-2 on nasopharyngeal sample testing. She provided a history of contact with a sick person at work.
On admission, she had a fever of 103.4 F, a heart rate of 124, and blood pressure 97/51 mm of Hg. Her oxygen saturation was 99 percent in room air. Her lab tests showed she had lowered white blood cell counts with a rise in lymphocytes and also had normocytic anemia. Her chest X-ray showed she had features of consolidation on both lungs. Typical features of “ground-glass opacities” were seen on CT scan of chest, abdomen, and pelvis. She also had an enlarged spleen.
For treatment, she had been given Hydroxychloroquine and a one-time dose of Tocilizumab and supportive therapy. She also received anticoagulant heparin for treatment. Soon after admission, she developed lethargy, and her mental status was altered. She was found to have cerebral edema on CT scan of her bread. MRI brain also showed “small acute infarct in the left temporo-parietal peri-ventricular white matter with a high medial right parietal cortical infarct,” the researchers wrote.
Her blood oxygen fell, and on day 3 of admission, she had to be intubated. On lab workup, it was found that she was “positive (for) anticardiolipin IgM and anticardiolipin IgG phospholipid antibodies”. She had normal levels of “Antithrombin III, Homocysteine level, Beta-2-glycoprotein 1 antibody, Protein C resistance, Factor V Leiden, MTHFR gene, and Calreticulin gene expression,” they wrote.
Case 2
The second case in the series was a 58 years old male who presented to the doctors with shortness of breath, fever, and dry cough. He had high cholesterol. On admission, he had no fever, and his blood pressure was normal with a raised heart rate. His chest X-ray showed a patchy appearance on both lungs. His nasopharyngeal sample also tested positive for SARS-CoV-2.
As a treatment, Hydroxychloroquine and Azithromycin were administered. On the sixth day, he was given interleukin-1 receptor antagonist, Anakinra. The same day it was noted that his left leg was colder than the right, and he was pale and cyanosed. The leg pulses on his left were also missing. This indicated a thrombotic event. For the treatment of acute peripheral artery disease, he was administered low molecular weight heparin (LMWH). He was investigated with an arterial Doppler study that showed no significant arterial occlusive disease. Still, a CT scan showed “absent flow distal to the left posterior tibial artery” and occlusion at the “left mid-peroneal artery and distal left anterior tibial artery.”
Lab work on the patient showed that he was also positive for anticardiolipin IgM and anticardiolipin IgG phospholipid antibodies. The authors suspected antiphospholipid syndrome (APS). Other markers such as “Beta-2-glycoprotein-1-antibody, JAK-2, and Calreticulin gene abnormal expression screens” did not show positive results they wrote.
Conclusions & Implications
Both of the cases reported in the study showed that thrombotic events were seen in the patients. They found clinically significant Antiphospholipid syndrome (APS). The team wrote in conclusion, “We believe our cases to be clinically relevant as they represent a new form of coagulopathy in SARS-CoV-2 patients. Further understanding of the complications associated with the disease can help our comprehension of the pathophysiology of the disease.” They said that it was unclear if anticardiolipin antibodies development could be due to the septic phase of the disease of APS. They suspect it could be due to the development of APS. The team calls for more studies to see the patterns of coagulopathy among COVID-19 patients to determine the clinical course of the infection as well as the possible therapy and management.
Journal reference:
- Sami Hossri, Mahmoud Shadi, Zaid Hamarsha, Rick Schneider, Dany El-Sayegh, Clinically significant anticardiolipin antibodies associated with COVID-19, Journal of Critical Care, Volume 59, 2020, https://doi.org/10.1016/j.jcrc.2020.05.017.