Researchers have presented the results of a large-scale coronavirus disease 2019 (COVID-19) testing program introduced across Oxford University Hospitals on 23rd April this year.
Staff who shared a household with an infected person were at the greatest risk of infection, and those working in COVID-19-facing areas were also at an increased risk. Other groups that were identified as a high risk included Black and Asian individuals, porters, and cleaners.
The researchers say the findings suggest that the provision of level-2 personal protective equipment (PPE) should be more widely deployed in settings where staff are at an increased risk of infection.
However, the transmission rate observed among workers who were at a less increased risk indicates that all staff need protecting, irrespective of their job role, adds the team.
A pre-print version of the paper is available in the server medRxiv*, while the article undergoes peer review.

Image Credit: BasPhoto / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Hospital workers still at greater risk following lockdown
On 23rd March 2020, the UK introduced lockdown measures to protect against the rapidly spreading severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19.
Although this involved a stay-at-home policy for most UK households, hospital workers had an occupational risk of infection through exposure to patients and other staff members.
Social distancing measures and the provision of PPE were introduced in hospitals to help mitigate occupational risk. However, the incidence of COVID-19 is still higher among healthcare workers than among the general population.
Walker and colleagues say that “crucial to designing a safe working environment and maintaining effective healthcare services is an understanding of the risks associated with specific roles and to individuals, and whether the risk is associated with social-mixing, direct exposure to Covid-19 patients or PPE type,”
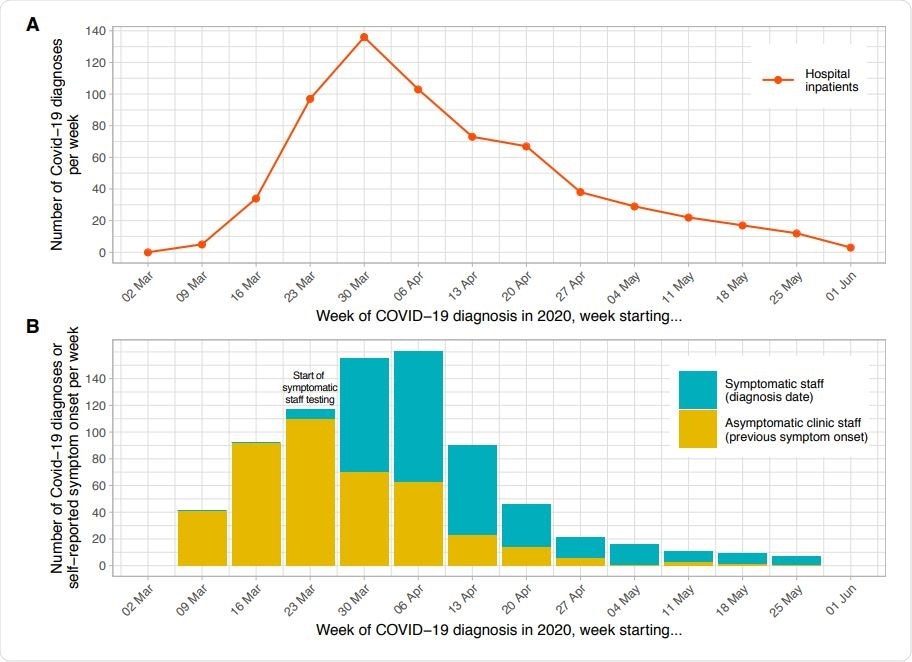
Epidemiological curve – hospital inpatients (panel A) and staff (panel B) diagnosed with Covid-19, by week. Each patient admitted to hospital with a diagnosis of Covid-19 within ±7 days of any day during their admission is plotted based on the date of their positive PCR test. Testing for symptomatic staff was made available from 27th March 2020; staff were asked to attend on day 2-4 of symptoms and are plotted in the week of their positive test. Of 1083 staff positive by PCR or serology at the asymptomatic staff clinic, 183 had been previously diagnosed at the symptomatic staff clinic. Of the remaining 900 positive staff, 472 (52%) reported a date when they believed a Covid-19 illness had begun, these are plotted in yellow above, many with symptoms before the availability of staff testing. As 428 (48%) of staff did not provide a date of symptom onset the true values for the yellow bars on the y-axis are likely to be around 2 times higher.
Comprehensive testing program introduced across Oxford University Hospitals
Walker and colleagues conducted a large, comprehensive testing program across Oxford University Hospitals NHS Foundation Trust, which spans four teaching hospitals run by a workforce of 13,800 and serving a population of 680,000.
A voluntary screening program was made available to all symptomatic and asymptomatic staff working at all sites across the hospitals.
Staff were tested using real-time PCR (polymerase chain reaction) of nasopharyngeal swabs and serologic analysis checking for antibodies against the virus. Data regarding potential risk factors for COVID-19 were assessed using multivariable logistic regression.
Which groups were at the highest and lowest risk?
Among 9,809 (71%) of staff who agreed to be tested, 1,083 (11%) showed evidence of SARS-CoV-2 infection.
The most significant risk was observed among staff living with an infected household member, although only 37% of these workers became infected. Higher rates of infection were also observed among staff working in COVID-19-facing areas than among staff working elsewhere, at 21.2% versus 8.2%.
Univariate analysis showed that staff who had the most direct contact with patients were at an increased risk, including cleaners, porters, healthcare assistants, nurses, junior doctors, and therapists.
However, once multivariate analysis controlled for working in a COVID-19-facing area, risks of infection varied across different working locations. People working in acute medicine were at a 50% greater likelihood of being infected, while staff working in COVID-19-facing ICU had a 54% lower likelihood of being infected.
The researchers say that one key factor that could explain this difference is the type of PPE provision, and when exactly it was mandated, level-2 PPE was mandatory throughout, whereas policies across other wards changed over time.
Furthermore, ICU staff received extensive training in “donning and doffing” and were provided with the space to do this, whereas other ward workers were not, adds the team.
Black and Asian individuals were at a 20% increased likelihood of testing positive for SARS-CoV-2, irrespective of their job role and working location, while porters and cleaners had a 93% greater likelihood of being infected.
“That staff working as porters or cleaners had the greatest adjusted risk of infection is consistent with economics playing a part in risk, potentially reflecting conditions outside of the hospital, e.g., dense occupancy of living space due to lower incomes,” explains Walker and colleagues.
What do the researchers advise?
The researchers say their findings suggest that earlier provision of universal level-1 PPE may have prevented some cases of infection and that the provision of level-2 PPE, training, and space for donning and doffing was protective among staff located in high-risk areas.
“Wider deployment of this bundle should be considered where staff are at increased risk,” advises the team.
The researchers say their findings could be used to inform staff risk assessments and ensure workers who are at the highest risk are managed accordingly.
“Given likely staff-to-staff transmission where COVID-19 patient pressure was low, there is a need to protect all staff regardless of role,” says the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Walker T, et al. Differential occupational risks to healthcare workers from SARS-CoV-2: A prospective observational study. medRxiv 2020. doi: https://doi.org/10.1101/2020.06.24.20135038
- Peer reviewed and published scientific report.
Eyre, David W, Sheila F Lumley, Denise O’Donnell, Mark Campbell, Elizabeth Sims, Elaine Lawson, Fiona Warren, et al. 2020. “Differential Occupational Risks to Healthcare Workers from SARS-CoV-2 Observed during a Prospective Observational Study.” Edited by Marc Lipsitch, Miles P Davenport, and M Estee Torok. ELife 9 (August): e60675. https://doi.org/10.7554/eLife.60675. https://elifesciences.org/articles/60675