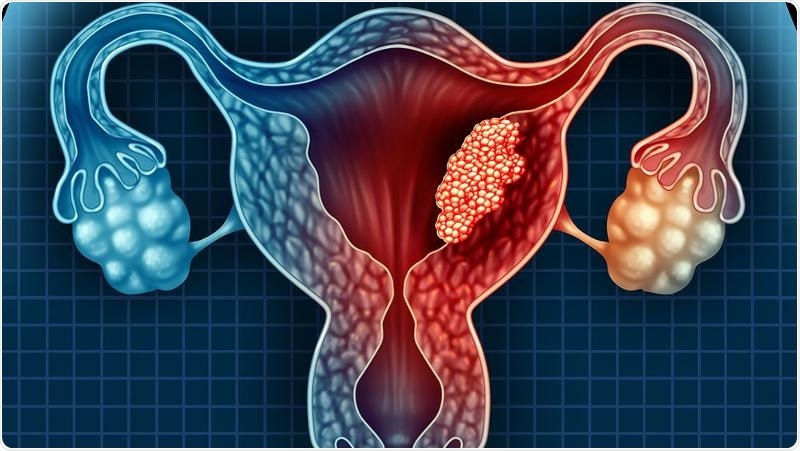
A newly discovered endometrial (uterine) cancer biomarker and diagnostic method will enable detection of the tumor type that is likely to spread and recur so that clinicians can initiate treatment early and stop the cancer from attacking other parts of the body.
- 3000 women in Australia a year diagnosed with endometrial (uterine) cancer
- New gene variant found that leads to one of the aggressive forms of this cancer
- This biomarker enables early detection and treatment to prevent cancer from spreading
- Biomarker could also be used to personalize anti-cancer therapy
The new biomarker could also be used to develop therapies to precisely target the cancer before it spreads to other parts of the body.
QUT Associate Professor Pamela Pollock and PhD student Asmerom Sengal from QUT Faculty of Health’s School of Biomedical Science, have developed and optimized a new technique to specifically detect a gene variant that leads to an aggressive form of endometrial or uterine cancer.
“The biomarker is based on a variation of the gene Fibroblast Growth Factor Receptor 2 (FGFR2) and we found it was expressed in 40 per cent of 386 patient tumor samples used in our study,” said Professor Pollock, who is based at the Translational Research Institute and a member of QUT’s Institute of Health and Biomedical Innovation.
We found this variant version of FGFR2 was linked with shorter survival and progression-free survival in a significant number of women. In my earlier research I was the first to identify mutations in FGFR2 that turned the protein on all the time, and this latest research builds upon that finding because we have found a new way that FGFR2 is turned on. Based on our findings, we believe thisvariation called FGFR2c, could be used both in the finetuning of prognosis for endometrial cancer, and also as a predictive biomarker that indicates whether the tumor will be sensitive to or resistant to FGFR inhibition.”
Pamela Pollock, QUT Associate Professor
Professor Pollock said FGFR2 was a viable therapeutic target in endometrial cancer as two FGFR inhibitors have now been approved in the United States for treatment of other cancers (bladder and bile duct cancers) that showed FGFR activation.
“We’d like to trial anti-FGFR therapeutics to treat women with high-risk uterine cancer, but first, we need to run critical pre-clinical trials.”
Professor Pollock said endometrial cancer was on the rise with 3000 women diagnosed in Australia a year, 80 per cent cases of which were associated with obesity.
There are two types of endometrial cancer - one that’s associated with obesity (Type 1) and overall has a better prognosis, and another one that represents 20 per cent of cases that is not associated with obesity and where FGFR2 doesn’t play an important role. Our test can detect the cancers within the generally ‘good prognosis’ obesity-related group that are likely to come back and will need targeted treatment to prevent recurrence and metastasis. This is important as this ‘good prognosis’ group still contributes to around 50 per cent of all deaths from endometrial cancer. Fortunately, 70 per cent of women with endometrial cancer are diagnosed early and after hysterectomy, and radiation if there is no spread, they are cured, and it won’t come back. Of the other 30 per cent of cases, 15 per cent will have a recurrence and 15 per cent will present with a cancer that has already spread outside the uterus. This new biomarker, FGFR2c will lead the way to detecting early the 10-15 per cent of women whose tumor is likely to recur and spread within a group that was previously thought to all have a good chance of survival.”
Pamela Pollock, QUT Associate Professor
Professor Pollock has received a $50,000 Perpetual grant from ANZGOG to validate the findings from this paper in a large international cohort of patients from a clinical trial.
FGFR2c mesenchymal isoform expression is associated with poor prognosis and further refines risk stratification within endometrial cancer molecular subtypes was published in Clinical Cancer Research.