The transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has long been associated with respiratory droplets when a person coughs, sneezes, or talks. Recently, evidence showed that SARS-CoV-2 virus particles can linger in the air as aerosols, making it spread faster.
Now, a new study by researchers at the University of Florida highlights the role played by SARS-CoV-2 aerosols in disease transmission.
Aerosol transmission
As the pandemic grows and spreads vastly across the globe, many scientists have suggested that aside from respiratory droplets, airborne transmission is possible in the spread of SARS-CoV-2.
Recently, the WHO said aerosol transmission is confirmed, especially in areas that are not well-ventilated. Previously, the WHO said that airborne transmission is only possible in hospitals via medical procedures that involved the release of aerosols, including nebulization and suctioning.
“WHO, together with the scientific community, has been actively discussing and evaluating whether SARS-CoV-2 may also spread through aerosols in the absence of aerosol-generating procedures, particularly in indoor settings with poor ventilation,” the WHO explained.
Aerosol transmission happens when several respiratory droplets produce microscopic aerosols, measuring about less than 5 µm, by evaporating and when a person breathes, coughs, sneezes, or talks. People could inhale aerosols, which can cause infection. Aerosols contain the virus in sufficient quantity to cause infection.
The study published on the preprint server medRxiv* shows that patients with respiratory symptoms of COVID-19 produce aerosols in the absence of aerosol-generating procedures that contain viable SARS-CoV-2. These aerosols can contain the virus and cause the transmission of the disease-causing pathogen.
The study
To arrive at their findings, the team collected air samples in the room of two COVID-19 patients, one of whom had an active respiratory infection with a nasopharyngeal swab positive for SARS-CoV-2. The researchers used VIVAS air samplers, and the samples were subjected to RT-qPCR and virus culture.
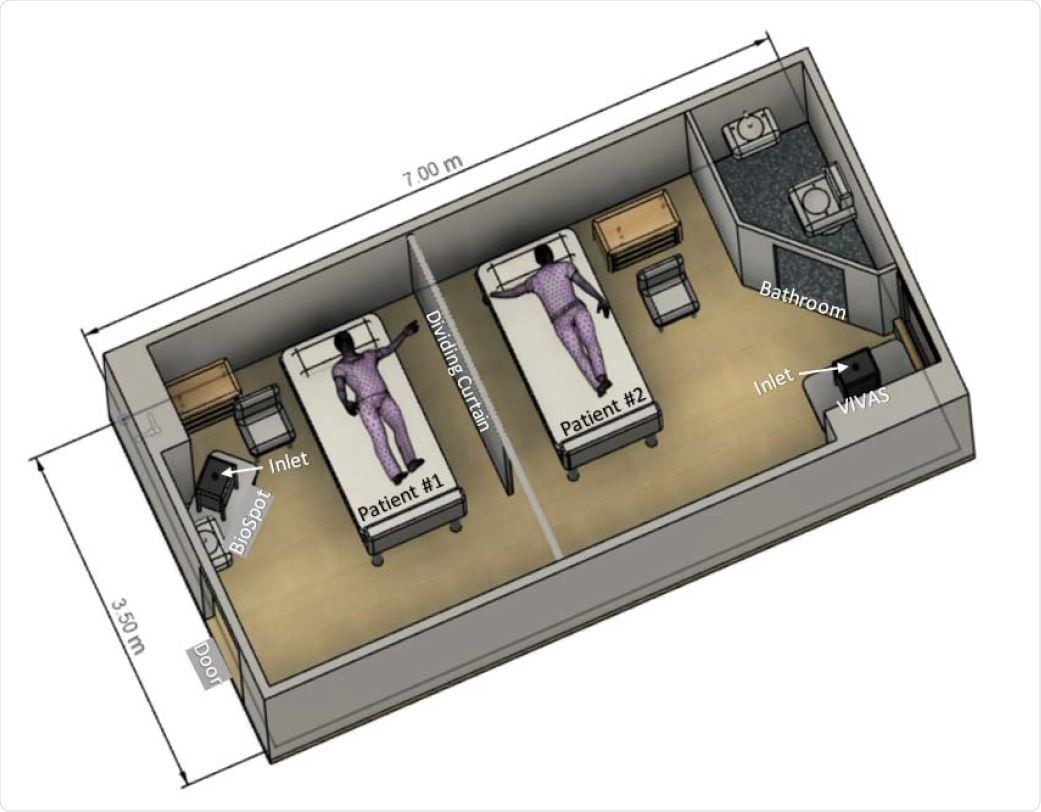
Schematic diagram of room with depiction of patient bed and air-sampler locations.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The findings of the tests revealed that a viable virus was isolated from air samples that were collected about 2 to 4.8 meters away from the patients. The genome sequences of the novel coronavirus strain isolated from the material collected by the air samples were identical to that isolated from the swab of the patient with active infection.
“Patients with respiratory manifestations of COVID-19 produce aerosols in the absence of aerosol-generating procedures that contain viable SARS-CoV-2, and these aerosols may serve as a source of transmission of the virus,” the researchers wrote in the paper.
The study findings shed light on how the virus can spread even in indoor spaces. The public health implications of the study are broad, especially that the current best practices to curb the spread of COVID-19 focus on wearing face-coverings or masks, social distancing, and frequent handwashing.
However, in airborne transmission, physical distancing by about six feet would not be enough to help in indoor settings. The researchers call for clear guidance on control measures against SARS-CoV-2 aerosols. This way, the spread of the virus, especially indoors, can be averted.
![Cytopathic effects in Vero E6 cells inoculated with material collected from the air during air sampling 1-1. [A] Mock-infected Vero E6 cells, 10 days post-inoculation with sterile collection medium. [B]. Large cytoplasmic vacuoles in Vero E6 cells inoculated with collection medium from BioSpot sample 1-1 at 4 dpi. [C] Early focus of infection 7 dpi. [D] Focus of infection 10 dpi. Rounded cells that are detaching, some in clumps, are present. Attached cells remaining in this focus of infection have dark cytoplasms, some have large cytoplasmic inclusion bodies, and some cells are elongated. Original magnifications at 400X. Cytopathic effects in Vero E6 cells inoculated with material collected from the air during air sampling 1-1. [A] Mock-infected Vero E6 cells, 10 days post-inoculation with sterile collection medium. [B]. Large cytoplasmic vacuoles in Vero E6 cells inoculated with collection medium from BioSpot sample 1-1 at 4 dpi. [C] Early focus of infection 7 dpi. [D] Focus of infection 10 dpi. Rounded cells that are detaching, some in clumps, are present. Attached cells remaining in this focus of infection have dark cytoplasms, some have large cytoplasmic inclusion bodies, and some cells are elongated. Original magnifications at 400X.](https://www.news-medical.net/image-handler/picture/2020/8/de.jpg)
Cytopathic effects in Vero E6 cells inoculated with material collected from the air during air sampling 1-1. [A] Mock-infected Vero E6 cells, 10 days post-inoculation with sterile collection medium. [B]. Large cytoplasmic vacuoles in Vero E6 cells inoculated with collection medium from BioSpot sample 1-1 at 4 dpi. [C] Early focus of infection 7 dpi. [D] Focus of infection 10 dpi. Rounded cells that are detaching, some in clumps, are present. Attached cells remaining in this focus of infection have dark cytoplasms, some have large cytoplasmic inclusion bodies, and some cells are elongated. Original magnifications at 400X.
What can be done
Understanding how, when, and in what types of settings SARS-CoV-2 spreads is essential to develop effective public health and infection preventive measures to contain the spread of the virus.
Currently, many countries practice health measures such as maintaining social distancing, wearing masks, washing hands regularly, and avoiding crowds due to the risk of COVID-19 infection. Respiratory droplets have been known as the main route of transmission. Still, with emerging evidence of airborne transmission, health experts recommend modifying these health measures, particularly in indoor spaces where there is limited ventilation.
Wearing of masks inside offices, workplaces, and groceries, among others, is very important to prevent the spread of the virus. Further, ventilation should be improved, while some experts say that letting natural air to come it can help reduce the virus spread.
Up to date, there are 18.73 million confirmed cases across the globe, with more than 706,000 deaths. Each day thousands of cases are being added, while other countries are reporting second waves of the virus. With lockdown measures being eased, it is crucial for people to be more cautious and vigilant to prevent infection.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Lednicky, J., Lauzardo, M., Fan, H., et al. (2020). Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patient. medRXiv. https://www.medrxiv.org/content/10.1101/2020.08.03.20167395v1
- Peer reviewed and published scientific report.
Lednicky, John A., Michael Lauzardo, Z. Hugh Fan, Antarpreet Jutla, Trevor B. Tilly, Mayank Gangwar, Moiz Usmani, et al. 2020. “Viable SARS-CoV-2 in the Air of a Hospital Room with COVID-19 Patients.” International Journal of Infectious Diseases 0 (0). https://doi.org/10.1016/j.ijid.2020.09.025. https://www.ijidonline.com/article/S1201-9712(20)30739-6/fulltext.