Even as the coronavirus pandemic spreads over the world, scientists are working hard to identify the factors that influence its spread and replication. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is composed of four major structural proteins, namely a nucleoprotein or N protein, the envelope or E protein, the transmembrane matrix glycoprotein or the M protein and the spike glycoprotein or the S protein.
The S protein has two functional subunits, S1 and S2. The S1 binds to the angiotensin-converting enzyme 2 (ACE2), which is the receptor for the virus. Following this binding, the S protein is cleaved by cellular proteases at the S1/S2 junction. This allows the fusion peptide in the S2 subunit to be exposed, allowing the viral and host cell membranes to fuse. This fusion leads to the entry of the virus into the cytoplasm of the host cell.
Either the endosomal or the cytoplasmic membrane may take part in fusion depending on the cellular proteases available. In fact, a variety of proteases including trypsin, endosomal cathepsin, transmembrane serine proteases like TMPRSS2, and furin, may take part in priming the CoV spike protein. Unlike SARS-CoV-2, which has a monobasic binding site, the SARS-CoV-2 protein has a multibasic site, which may also be a furin cleavage site. Many betacoronaviruses can be activated by furin at the S1/S2 interface. Still, the SARS-CoV and the murine hepatitis virus strain 2 are exceptions that lack this site, and therefore require other cellular proteases for priming.
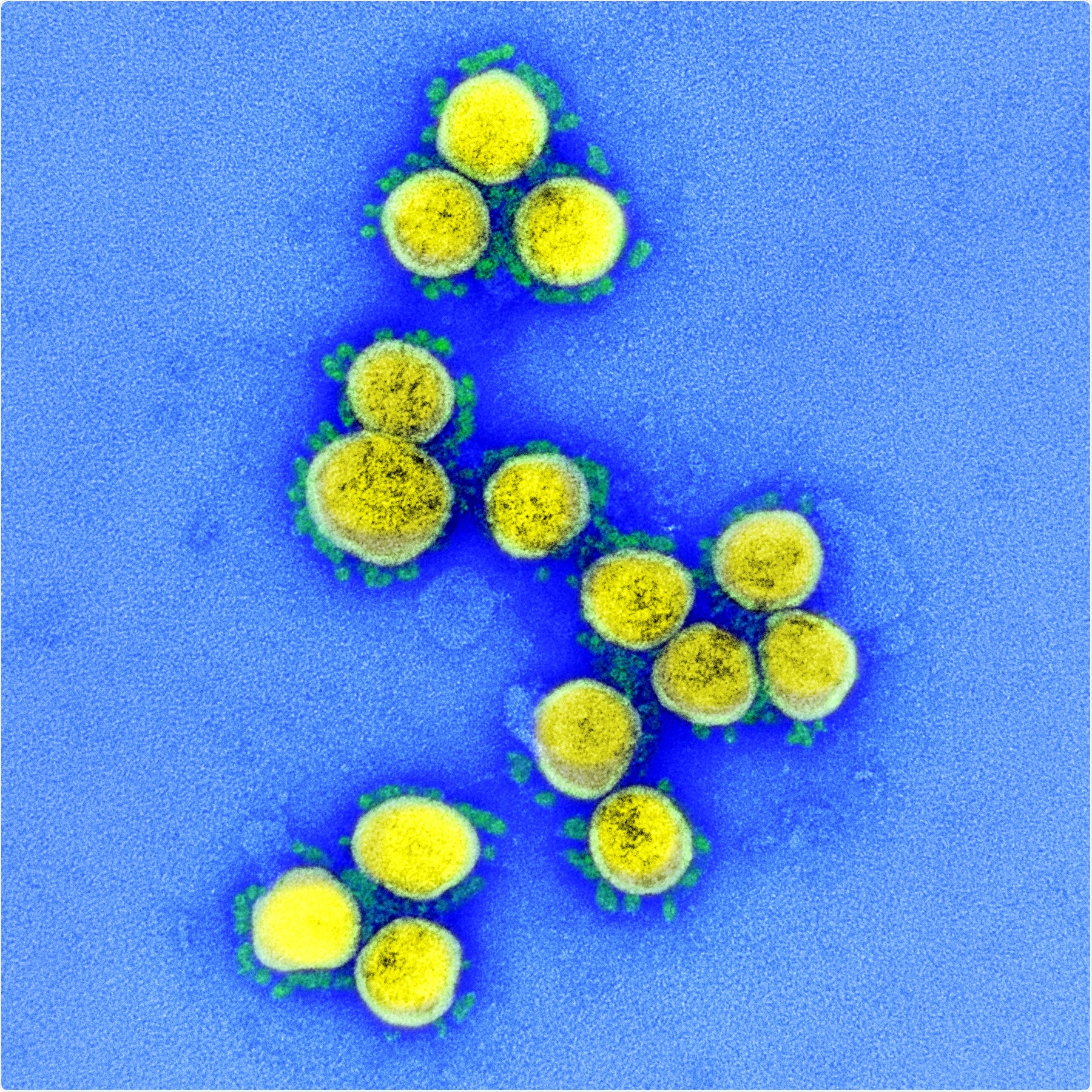
Novel Coronavirus SARS-CoV-2 Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Heparan Sulfate Binding Site
However, the furin recognition sequence in the SARS-CoV-2 spike protein is identical to the putative heparan sulfate (HS) recognition sequence though in the opposite orientation. Prior research shows that the Sindbis virus in cell culture can bind to HS via this site. The same characteristic is often seen when CoVs are cultured in vitro. Apparently, some CoVs can adapt themselves to heparan sulfate as a receptor in order to enter cultured cells.
Viral Quasispecies and Adaptation
An earlier study described the emergence of mutant forms of the SARS-CoV-2 with deletions at the S1 /S2 interface upon culturing in Vero E6 cells. It is well known that RNA viruses can rapidly adapt because of the presence of viral quasispecies. Currently, circulating SARS-CoV-2 isolates have shown furin mutations in the recognition sequence. Now a new study published on the preprint server bioRxiv* aims to explore the presence of such quasispecies and how they help the virus to adapt to changes in the environment.
Quasispecies are different genome variants present in abundance in a population of a given RNA virus. They originate as a result of proofreading errors of RNA-dependent RNA polymerase (RdRp). They are a source of adaptive mutations contributing to the fitness of the virus.
The current study shows that SARS-CoV-2 is a quasispecies that possesses a very stable genome overall. However, this property is primarily due to the complex apparatus used for RNA synthesis and the key enzyme exoribonuclease (ExoN) that maintains genomic stability. When this is mutated, the mutation frequency of the genome increases tenfold.
The presence of virus quasispecies enables it to rapidly adapt to antiviral compounds or to biological drugs that target a specific molecular site in the proteome. This would help escape or resistant mutants to emerge, and so put virus control beyond reach.
Selective Mutations via Passaging
In this new study, the virus was serially passaged in independent cell types in a controlled environment. The researchers found that the virus rapidly adapts to the changing conditions in culture by selecting for pre-existing species.
The researchers found a viral point mutation occurred in Vero cells resulting in the loss of the furin cleavage site PRRARS at the S1/S2 junction, with a 15 base pair deletion. The genomes of different isolates were stable overall even after several passages, but the furin cleavage site rapidly develops mutations on passaging.
One of the strains developed multiple point mutations resulting in the loss of two arginines. Another strain showed a specific mutation In this protein in 85% of the passage 3 genomes. In short, all strains showed rapid mutation at this site, with a small percentage retaining the wild type furin site. The researchers summed up, “Overall, our data demonstrated that the furin cleavage site was rapidly mutated upon SARS-CoV-2 culture in Vero E6 cells, but it was not completely lost. Virus genomes with wildtype furin sites were retained as subdominant variant in the population.”
High Passage Strains Grow on Vero Cells, not Calu-3 Cells
High passage strains grow better on Vero E 6; however, this was not due to better viral release from infected cells but rather due to an early event after infection. On TMPRSS2-positive Calu-3 cells, the early assessment showed improved growth of low-passage viruses. This confirms prior findings that the multibasic site is necessary for the cleavage of this protein by TMPRSS2.
Fusion Cleavage Site Restored When Grown in TMPRSS2 Cells
TMPRSS2-positive cells thus give cells with the wildtype furin cleavage site a growth advantage. The researchers took the NK strain that had lost this site after six passages in Vero E6 cells and passaged it again on Calu-3 cells instead. They found that reverse mutation occurred, with the furin site reverting to the wildtype.
The high-passage virus showed initial slow growth, which then rapidly picked up, comparable to the low-passage virus. The reverse mutation occurred predominantly in the first passage, with the mutant genomes being the subdominant strain. The composition of the NK6 virus quasispecies was thus altered to show a reverse mutation rate of 0.63 and a mutation rate of 0.01.
The results indicate that targeted evolution and not genetic drift is at work. If the latter, the loss of it would fail to select the cell clones that lack the proteases, though its presence would improve growth on cells that have furins to cleave this site.
Unexpected Mutations May Confuse Results
The low-passage virus swarm retained a stable genome composition on either Calu-3 or Caco-2 cells, whatever the earlier mutations that had occurred while passaging on Vero cells. In Calu-3 cells, however, new E protein mutations emerged during passaging, but not on Vero E6 cells. This improved viral growth in Calu-3 but not Vero cells.
Again, the emergence of different mutations and reverse mutations when the virus is grown on different cell lines shows that none is the best to maintain the stock virus. Indeed, mutations are acquired in high-passaged strains that could confuse results obtained with them.
The Furin Cleavage Site and Viral Entry
The researchers further tested the growth of high- and low-passage viruses in the presence of inhibitors of TMPRSS2, furin, or a broad-spectrum endosomal protease inhibitor. The latter inhibited the growth of all strains in Vero cells, and the others had no additive effect. This shows the crucial role of the endosomal rather than the cell surface protease for replication. The mutation in the high-passaged virus probably occurred at the time of virus entry.
In the Calu-3 cells, the TMPRSS2 inhibitor reduced the growth of all strains to equal titers. With all three inhibitors, viral growth stopped, indicating protease redundancy. In Caco-2 cells, however, normal replication continued with a single inhibitor but stopped with a combination of inhibitors. Thus, the researchers say, “Our results indicated that the inhibition of virus entry into cells by protease inhibitors abrogated the growth advantages conferred by differences at the furin recognition site.”
Heparan Sulfate Binding Enhances Viral Growth in Vero Cells
Mutations in the HS binding site reduce its positive charge but enhance its hydrophobicity. This site overlaps with the furin cleavage site. When treated with an HS inhibitor, low-passage strains increased tenfold. However, this failed to occur if the HS site mutation was present. This was confirmed with plaque tests.
In other words, when the HS binding site is lost, viral growth improves, perhaps because HS-virus binding to the cell surface prevents its internalization via endosomes. Or it might cause steric inhibition of endosomal proteases, which find their recognition site at the monobasic sequence at the S1/S2 interface.
Implications
The researchers comment: “These observations suggest that SARS-CoV-2 maintains a considerable diversity in the quasispecies, facilitating natural selection and a rapid virus adaptation to changing environment and conditions.” Since individual viruses are less fit, rapid adaptations help the viral swarm to be more fit overall.
The use of antiviral monotherapies could lead to rapid selection of subdominant pre-existing species allowing resistance to emerge to the mode of action of the specific compound. Another type of oligoclonal immune response may cause escape mutants to arise with changes at a few epitopes only. This type of immune response is seen in older people and may contribute to severe disease in this age group. Thus, the researchers say, “Our research indicates that the presence of subdominant genetic variants within SARS-CoV-2 isolates needs to be considered as a potential determinant of their virulence.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources