In the view of the ongoing coronavirus disease 2019 (COVID-19) outbreak, SARS-CoV-2 has shown a varied level of genetic heterogeneity and disease severity worldwide. The virus has also been shown to severely affect older adults and people with comorbidities, leaving healthy children and young adults in a relatively safer position.
Given these differential viral responses, it is generally hypothesized that having a previous history of infection or immunization against common alpha coronaviruses (HCoV-NL-63 and -229-E) and beta coronaviruses (HCoV-OC-43 and -HK-U1) may provide cross-protection against SARS-CoV-2.
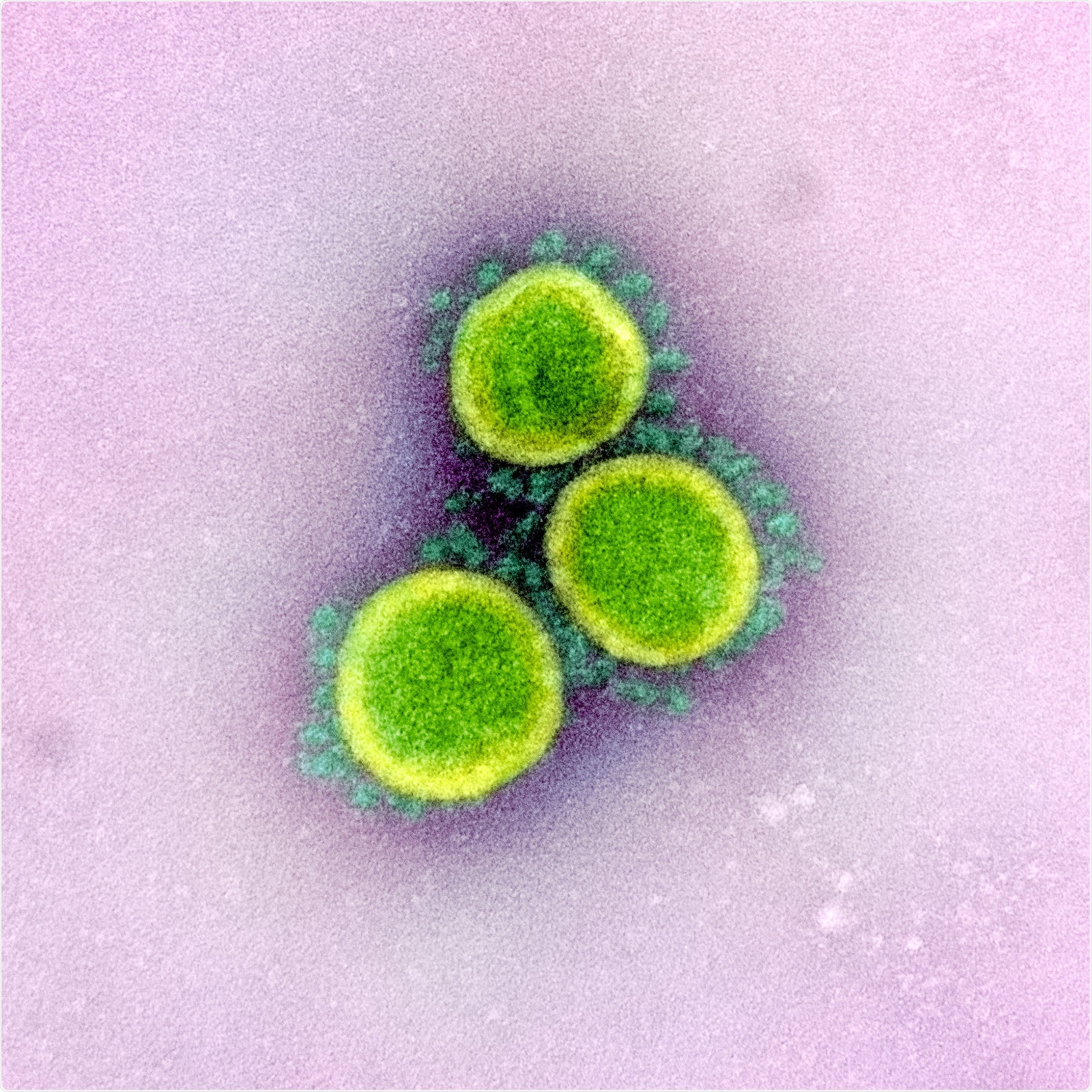
Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The present study designs
To verify this hypothesis, the scientists of the current study analyzed serum samples collected from 76 healthy individuals before the outbreak of COVID-19. Interestingly, the scientists found that about 8% of serum samples have cross-reactivity against several SARS-CoV-2 antigens, including S2 domain, full-length spike protein, nucleocapsid. However, no cross-reactivity against receptor binding domains (RBDs) of the viral spike protein was observed. In addition, these serum samples showed random cross-reactivity against all types of common coronaviruses. From these observations, the scientists concluded that immunity developed in the pre-COVID era show only nonspecific reactivity to SARS-CoV-2 antigens.
For further verification, the scientists checked the reactivity of therapeutic intravenous immunoglobulin G (IgG) formulations, which were manufactured before the COVID-19 pandemic. These intravenous formulations, which are composed of IgG molecules isolated from 10,000 pooled plasma samples of healthy individuals, are expected to provide valuable information about pre-existing adaptive immune response of the general population.
Using three different sets of intravenous formulations, the scientists observed significantly high IgG reactivity against all types of common coronaviruses and detectable IgG reactivity against different SARS-CoV-2 antigens, including full-length spike protein and S2 domain. However, no reactivity against nucleocapsid was observed. From these observations, the scientists concluded that the adaptive immunity developed before COVID-19 pandemic commonly shows cross-reactivity against SARS-CoV-2 antigens in the general population.
Determining the bidirectionality of cross-reactivity
To determine whether antibodies developed against SARS-CoV-2 can react to both SARS-CoV-2 and common coronavirus antigens, the scientists analysed IgG reactivity of serum samples collected from eight severely affected COVID-19 patients against antigens of both SARS-CoV-2 and common coronaviruses. The scientists observed an increase in antibody titers (IgG) against SARS-CoV-2 and beta coronavirus antigens. Because the patients tested positive only for SARS-CoV-2 and not for other coronaviruses, the scientists believed that these IgG responses against beta coronavirus are possibly a result of cross-reactivity.
The scientists also observed that early serum samples collected from patients were reactive to beta coronavirus; also, serum samples of two patients were reactive to alpha coronavirus. All these immune responses occurred even before the appearance of antibodies against SARS-CoV-2. From these observations, the scientists believed that developing immunity against common coronavirus infection cannot protect individuals from developing COVID-19. Their assumption was further established by a series of in vitro assays showing that pre-COVID serum samples without detectable levels of anti-RBD antibodies failed to neutralize SARS-CoV-2. Similarly, intravenous IgG formulations prepared before the SARS-CoV-2 pandemic did not show any neutralizing effects.
Taken together, the scientists proposed that although cross-reactivity happens between SARS-CoV-2 and common coronaviruses, cross-protection against SARS-CoV-2 can be achieved only from antibodies developed against SARS-CoV-2. Lack of cross-protection may be due to not having structural similarity between RBDs of SARS-CoV-2 and common coronaviruses. Structural homology between the S2 domains of SARS-CoV-2 and common coronaviruses is responsible for cross-reactivity, but fails to provide cross-protection.
Another important observation made by the scientists is that intravenous IgG formulations developed before the SARS-CoV-2 pandemic do not hamper the neutralizing ability of patient-derived serum IgG against SARS-CoV-2. This observation indicates that people who have recovered from SARS-CoV-2 infection should not be excluded as donors for preparing intravenous IgG formulation during the COVID-19 pandemic. However, one crucial thing to be taken into consideration is that serum IgG samples from these donors should not amplify the infection instead of nullifying it (antibody-dependent SARS-CoV-2 enhancement activity).
Because it is still not established whether plasma samples obtained from people recovered from COVID-19 are effective in treating SARS-CoV-2 infected patients, the scientists believed that intravenous IgG formulations developed during the COVID-19 pandemic are not supposed to play any therapeutic roles. However, these formulations may have prophylactic effects against SARS-CoV-2 infection.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources