Since late December, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread from Wuhan, China, to all continents, causing a severe pandemic. Globally, as of today, there are over 23.75 million confirmed cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and over 815,000 related deaths. In Austria, the first cases were detected on February 25, 2020, and until early March, only a few limited outbreaks were observed.
The first case in Austria was on February 25, 2020, followed by small-scale outbreaks until early March. This peace was shattered by an explosive spreading event originating in the Austrian resort Ischgl, from where transmission occurred throughout Austria as well as many other countries the world over. Epidemiologists working with the Austrian Agency for Health and Food Safety (AGES) have estimated that up to 40% of cases in Austria began at Ischgl.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The ski bar at which spread occurred was closed on March 8, 2020, and all other apres-ski bars as well in the town on March 10. The valley, once cleared, thus remained free of tourists and guest workers for 6 weeks before the current study began, presenting an isolated population.
The researchers carried out a cross-sectional survey over the whole population of Ischgl, covering 79% of the population, including over 101 children under the age of 10 and 113 participants between 10 and 17 years. They performed a SARS-CoV-2 PCR, antibody test, and structured questionnaires. This was followed by mathematical modeling to understand the effect of the observed seroprevalence on viral spread.
Seroprevalence
The researchers showed that of about 1,470 individuals, from about 480 households, 624 individuals were seropositive in at least 2 of up to 4 antibody tests performed (3 binding antibody assays and 1 neutralizing antibody test). That is, the seroprevalence was 42.4%. This is a record high among reported seroprevalences so far, including that of New York City when the population is considered rather than patients only. It contrasts with the 5% seroprevalence found in many other hotspots outside Tyrol but in Austria, confirming that this was the epicenter of the European epidemic.
Immunoglobulin G (IgG) antibodies targeting the spike protein (anti-S) and nucleoprotein (anti-N) of SARS-CoV-2 correlated well in concentration. All serum samples which reported positive in one of two assays were positive for neutralizing antibodies also, and the anti-S IgG ELISA also showed a correlative trend with the neutralizing antibody titer.
The study shows that children and adolescents have significantly lower seroprevalence relative to adults, at 27% and 45%, respectively. This is thought to reflect the higher exposure, as, during tourist season, most people in Ischgl who are above 18 begin to work with the tourists. It is estimated that approximately 10,000 new tourists come in each week, while several hundreds of guests arrive from other ski resorts to the apres-ski bars in Ischgl. There was no difference between the sexes.
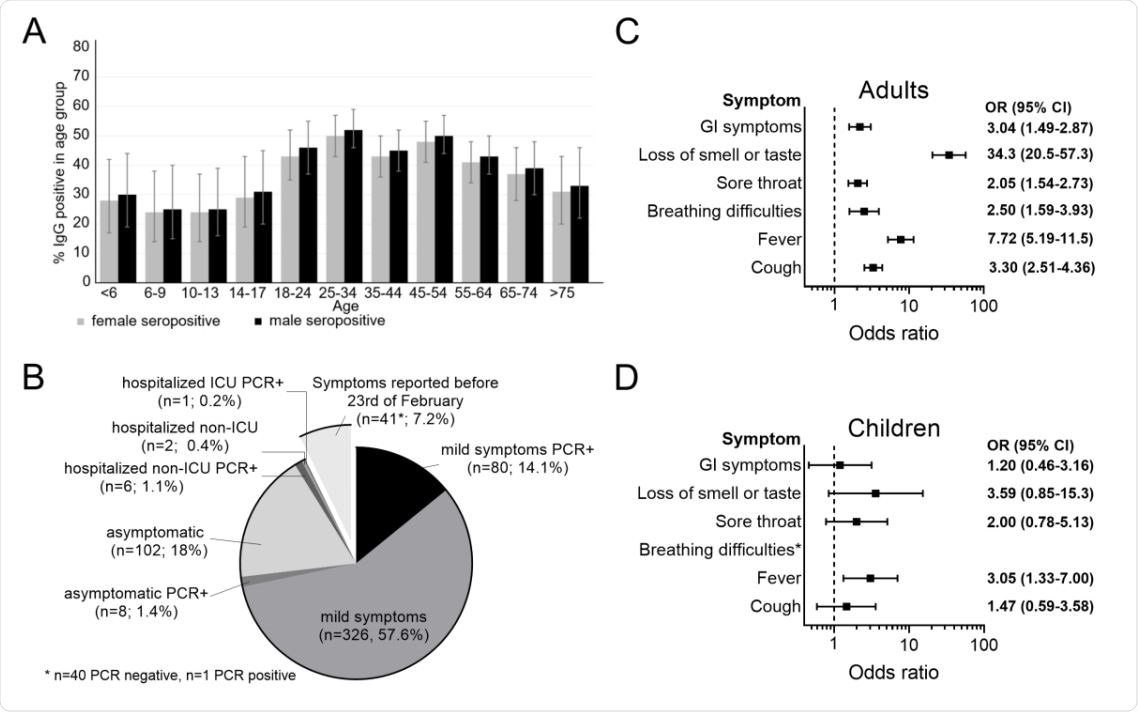
Seroprevalence and clinical course. The seroprevalence in different sex and age groups was calculated using a generalized estimating equation (GEE)-model taking household clusters into account (A). Clinical courses of COVID-19 in seropositive individuals were classified based on the information provided by the study participants. Mild disease was defined as reported COVID-19-associated symptoms not requiring hospitalization. Additionally, all study participants were asked if a SARS-CoV2 PCR was carried out and its result. Symptoms reported before February 23 were excluded as the peak of the influenza season was in the first half of February and the OR for reported symptoms and SARSCoV-2 seropositivity were low then (B). Odds ratios of self-reported symptoms regarding seropositivity in adults were calculated using generalized estimating equation (GEE)- model adjusted for age and sex, taking household clustering in account (C). Odds ratios of self-reported symptoms and symptoms reported by persons of care and custody, respectively, regarding seropositivity in children were calculated using generalized estimating equation (GEE)-model adjusted for age and sex, taking household clustering in account (D).
RT PCR Positivity
Nasopharyngeal swabs were positive on RT PCR in only 9 individuals or 0.6% of the participants. All 9 were asymptomatic and showed low viral loads. Eight of them were new cases and had neutralizing antibodies, four individuals had a history of symptoms, but the latest was 39 days before the study began. Anosmia and ageusia were present in three patients. The researchers conclude that viral RNA can be detected over long periods and even in the presence of neutralizing antibodies.
The very low prevalence of new cases from about 20% in a voluntary public screening of about 230 individuals to 0.5% in the current study, just 3 weeks later.
Prior to the study, 105 participants had undergone PCR testing with a positive result, and 102 (97%) of them had seroconverted by the time of the study. This shows that of the total 624 individuals who showed seroconversion, only 105 had been reported previously as having tested PCR positive. This means that up to 84% of non-diagnosed infections were picked up by serology in a hotspot, and one which was the epicenter of the Austrian epidemic. In children up to 18 years, only 10% were previously diagnosed, vs. 17% in adults.
These figures support some earlier studies, such as one from Germany based on serology, with a low infection fatality rate of 0.3%. The hospitalization rate was only 1.5% here, vs. the national rate of 15%. This could be due to the high proportion of unreported cases, and the lower seroprevalence in older patients. This suggests that more testing is required in hotspots to contain viral spread more effectively in the future.
Clinical Features
Cases reported after February 23, 2020, had a greater correlation with the development of antibodies, probably because the overlap of clinical symptoms with influenza was over by that point. Most participants had a mild or asymptomatic disease. Only 9 adults (0.6%) were hospitalized, in all.
Most participants remembered only mild symptoms, but anosmia/ageusia was highly predictive of IgG positivity, as well as fever and cough, to a much smaller extent. The odds for seroconversion were 34 times higher with the former, but 8 and 3 times higher with the latter. Children had variable correlations between symptoms and seropositivity.
There were two deaths in Ischgl due to COVID-19, both after March 20, 2020. This would give an infection fatality rate of 0.34% using the number of detected seropositive, and 0.25% if using the number of seropositive living in Ischgl. However, this is a purely theoretical and insignificant estimation as the number of deaths was very small.
Household Clusters
The entire household was seronegative in 39% of households, as well as having both seronegative and seropositive individuals in the same proportion. Among those which contained children (124), two-thirds had no positive children, but half had one or more positive adults. However, when children were positive, one or more adult in the households was almost invariably positive as well. Overall, the odds of infection in children were 66% lower than for adults when both were in the same household.
Implications
The researchers consider that the containment of the epidemic at present is not due to the reduction in reproductive number Re but due to the non-pharmaceutical interventions (NPIs) now in place. If all these strategies are relaxed, the viral transmission may begin again. However, there are some uncertainties, such as how far innate immunity contributes to the containment of the virus, even without specific antibody production. This could lead to the individual (especially a child) remaining apparently uninfected and seronegative, despite having encountered the infection. Thus, both the seroprevalence and the NPIs explain how the outbreak was limited.
Since herd immunity levels have not been met, continued NPIs must be implemented to keep the outbreak under control in Ischgl. Opponents of lockdown may, however, point to the absurdly small number of hospitalizations and deaths to underline the importance of aiming at herd immunity rather than NPIs to hasten the extinction of the pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources