COVID-19 disease is primarily characterized by fever, cough, and respiratory symptoms. However, it is also now known to affect many other organs, especially the gut. In fact, up to 60% of hospitalized patients present with gut symptoms. A new study by researchers at the Icahn School of Medicine at Mount Sinai and published on the preprint server medRxiv* in September 2020 shows that gut infection with this virus produces primarily mucosal immunity but also a limited inflammatory response.
Prior studies have described the presence of intestinal inflammatory markers in COVID-19 patients with diarrhea, such as stool calprotectin, a neutrophil protein which is measured as a marker of inflammatory bowel disease. COVID-19 patients also show marked changes in the fecal microbiome, suggesting that the infection disrupts the gut mucosal immunity.
The host cell receptor for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the angiotensin-converting enzyme 2 (ACE2), is abundant on the epithelium of the small intestine, with viral RNA shedding occurring for long periods in the stool. Human gut organoids have also been found to be infected by the virus. This suggests the possibility of viral replication in the gut and transmission via feces.
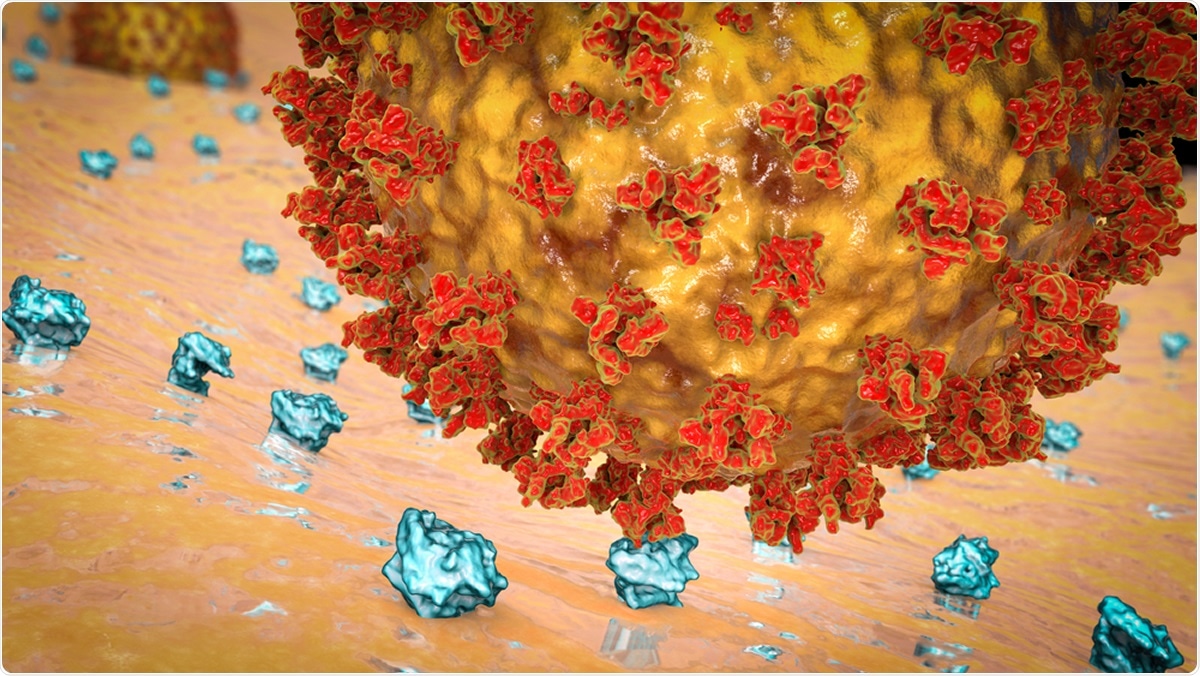
SARS-CoV-2 virus binding to ACE2 receptors on a human cell. Illustration Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Severe COVID-19 is associated with a significant imbalance of systemic immunity, and the blood levels of immune cytokines like interleukin (IL)-6, IL-8, IL-10, and tumor necrosis factor (TNFα) increase with increasing disease severity and worsening outcomes. The current study focuses on understanding how the virus affects the gut and its local immune responses as well as the fecal microbiome.
The study uses data from hospitalized patients in a single hospital in New York City at the peak of the pandemic. Stool samples were collected in the acute and convalescent phases of the infection, at a median of 16 days and 25 days, respectively, from symptom onset. The median patient age was 56 years, and while half of the patients were defined as obese, 70% had high blood pressure. About half were males.
Moderate and severe disease at presentation occurred in half and one-third of the patients, respectively. While those who were mildly ill at presentation continued to be so, half of those in the moderate category progressed to severe illness. About 16% and 30% of the patients died and were admitted to the intensive care unit (ICU) during their stay. Altogether, there were 14 patients, or 32% of the total, who required ICU care and/or died, this being taken as the poor composite outcome.
The researchers gave preference to those who presented with gut symptoms, and thus these patients made up about 70% of the cohort, mostly diarrhea in about 60%, nausea in a third, and vomiting in a sixth. The median age of patients with GI symptoms was younger than for those without, at 53 years vs. 63 years. Other ethnic, comorbidity, and severity/mortality data were similar in both groups. However, more patients without gut symptoms required ICU admission, at 54%, vs. 19% in those with such a presentation.
Inflammatory markers like serum IL-6 and IL-8 were lower in those with gastrointestinal (GI) symptoms, though this was not statistically significant. Other parameters relating to white cell count, lymphocyte count, and markers like CRP, LDH, D-dimer, and ferritin, as well as liver enzymes, were similar in both groups.
As the disease neared its peak, serum IL-6, IL-8, and TNF-α levels rose, as did CRP, LDH, D-dimer, and ferritin, but not liver enzymes.
Viral RNA in Stool Increases with Diarrhea and Fatal Disease
The researchers carried out quantitative PCR (qPCR) on the SARS-CoV-2 genome, using the cycle threshold Ct less than 40 as a positive result. They found that fecal PCR for viral RNA detection was positive for 41% of the patients. Higher loads were associated with the diarrheal presentation.
They also observed that RNA detection was most likely within 28 days from symptom onset, but within this period, there was no difference in detection rate based on the time point. No patient with a negative nasopharyngeal PCR result had detectable viral RNA in feces, though the median period between the negative nasal PCR and the stool sample collection was 11 days.
High Fecal Viral Load Marks Fatality of Infection
The researchers also found that non-survivors had much higher viral loads in feces than survivors, but the fecal Ct value was not proportional to disease severity. Moreover, of the very few patients with mild disease that were recruited to this study, half had detectable viral RNA in their feces.
Genome sequencing showed that each isolate belonged to clade 20C, which was circulating most freely in New York City at this time. No specific mutations linked to GI infection were observed.
Inflammatory Cytokines in Feces Of COVID-19 Patients
The investigators observed that fecal cytokines were elevated in COVID-19 patients, as in other intestinal infections and inflammatory conditions, but did not associate with GI infection or with diarrhea. This included higher IL-8, IL-1b, and TNFα levels, in some but not all the patients.
When sorted by disease severity, they found that only IL-23 was significantly increased in severely ill COVID-19 patients. Higher cytokine concentrations in serum were not reflected in stool concentrations; however, the value of this observation is limited since the specimens were not collected on the same days.
The level of calprotectin in feces was not linked to COVID-19 severity or the stool viral load.
Gut Microbiome Changes Unrelated to COVID-19
The researchers also found that there were no specific changes in the gut microbiome in COVID-19 patients. However, recent antibiotic therapy was associated with changes in the composition and reduced diversity of gut bacteria.
Gut-Specific SARS-Cov-2 IgA In COVID-19 Patients
The host immunity against SARS-CoV-2 is thought to depend heavily on neutralizing antibodies against the viral spike protein, particularly the receptor-binding domain (RBD). Mucosal immunity is mediated mainly by IgA antibodies, which are responsible for durable immunity against intestinal viruses.
Anti-SARS-CoV-2 IgA has been found in blood, bronchoalveolar lavage fluid, and nasal washes, as well as in breast milk from convalescent donors. The researchers, therefore, looked for anti-RBD IgA antibodies in fecal samples. They found that this was correlated with RBD-specific IgA in serum, but at a lower level.
The levels of total and RBD-specific IgA in stool across the group were broadly similar to that of healthy controls. There were 5 patients, all with severe COVID-19, who had substantial levels of specific IgA. Still, all were obese, with a median BMI of ~41 compared to 29 for other patients without detectable specific IgA.
Implications
The researchers suggest that based on this data, diarrhea in some COVID-19 patients is not the result of inflammation. However, the presence of GI symptoms typically indicates a milder course of the disease, but in severe cases, the immune dysregulation results in massive viral replication within multiple organs.
Fecal IL-8 elevation, coupled with lower IL-10 in COVID-19 patients, and higher IL-23 in severely ill patients, demonstrate an immune response within the gut to this viral infection. However, the fact that the viral load in stool does not reflect the severity of disease and the lack of involvement of other cytokines and of calprotectin shows that this is limited.
This is supported by the lack of changes in gut microbiome structure or diversity, except those that could be traced to the use of antibiotics.
Finally, the presence of RBD-specific IgA in stool has been detected for the first time in COVID-19 patients. However, it remains unclear whether this is a localized protective mucosal response or part of the systemic response to the infection. They discovered that fecal detection of specific IgA is difficult because of the high background noise, which demonstrates the need for more sensitive methods to pick up low titers.
The study concludes, “Our data suggest that the gut can be an immunologically active organ during SARS-CoV-2 infection, as evidenced by virus-specific IgA, but there is little evidence for overt intestinal inflammation, even in patients with diarrhea or other GI symptoms.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Britton, G. J. et al. (2020). SARS-CoV-2-Specific IgA And Limited Inflammatory Cytokines Are Present In The Stool Of Select Patients With Acute COVID-19. medRxiv preprint. doi: https://doi.org/10.1101/2020.09.03.20183947. https://www.medrxiv.org/content/10.1101/2020.09.03.20183947v1
- Peer reviewed and published scientific report.
Britton, Graham J., Alice Chen-Liaw, Francesca Cossarini, Alexandra E. Livanos, Matthew P. Spindler, Tamar Plitt, Joseph Eggers, et al. 2021. “Limited Intestinal Inflammation despite Diarrhea, Fecal Viral RNA and SARS-CoV-2-Specific IgA in Patients with Acute COVID-19.” Scientific Reports 11 (1): 13308. https://doi.org/10.1038/s41598-021-92740-9. https://www.nature.com/articles/s41598-021-92740-9.