Researchers in the United States have found that individuals who develop more severe disease following infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mount a larger antibody and memory B cell response during both acute infection and convalescence.
The team also found that the antibody response mainly targets two structures found on the surface of SARS-CoV-2, namely the spike protein and the nucleocapsid (N) protein.
The spike protein is the structure the virus uses to bind to and fuse with human host cells, while the N protein is needed for the synthesis of viral RNA.
Study participants who exhibited a greater antibody response also mounted a more significant memory B cell response against the spike protein than the N protein.
The team says the study shows that individuals with more severe SARS-CoV-2 infection have a more significant overall antibody response to the spike and N protein and a larger memory B cell response against spike.
A pre-print version of the paper is available on the server bioRxiv*, while the article undergoes peer review.
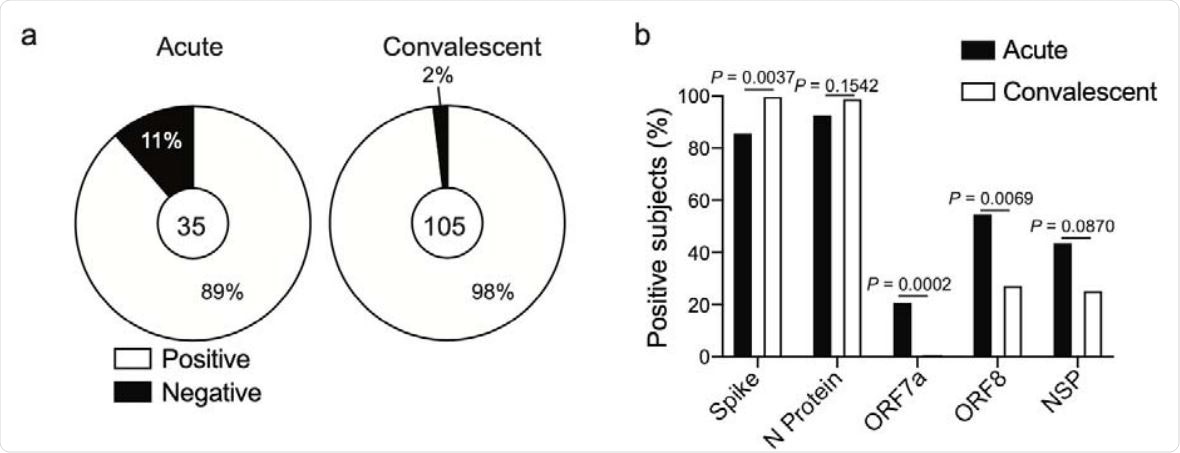
Antibody specificity and kinetics in SARS-CoV-2 infected subjects. a, Proportion of subjects in the acutely infected and convalescent cohorts who have seroconverted to one or more SARS-CoV-2 antigens. Number in center represents the number of subjects tested in each cohort. Proportion of subjects in the acutely infected (n=35) and convalescent (n=105) cohorts binding spike N protein, ORF7a, ORF8, or at least one NSP antigen.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Little is understood about the antibody response to SARC-CoV-2
SARS-CoV-2, the agent that causes coronavirus disease 2019 (COVID-19), displays various surface antigens, including two structural proteins other than Spike and N (envelope and matrix proteins); 16 nonstructural proteins (NSP1–NSP16), and several accessory open reading frame (ORF) proteins, including ORF7 and ORF8.
To date, little is understood about the specificity and kinetics of the antibody response mounted against the novel SARS-CoV-2 virus or how the severity of COVID-19 relates to the magnitude of the humoral immune response.
To address this crucial knowledge gap, Patrick Wilson (University of Chicago) and colleagues collected plasma samples from 35 hospitalized patients with acute SARS-CoV-2 infection 105 convalescent individuals.
Plasma was tested for SARS-CoV-2 -specific antibodies against the spike and N protein, as well as ORF7a, ORF8, and NSP3, NSP9, NSP10, and NSP15.
The team reports that 89% of patients with acute infection and 98% of convalescent individuals had detectable levels of antibodies against at least one SARS-CoV-2 antigen and that almost all subjects had antibodies against the spike and N proteins.
Comparing responses between acutely infected and convalescent individuals
Convalescent individuals mounted a predominant response to spike RBD and the N protein, while a larger proportion of patients with acute infection launched a response against ORF7a, ORF8, and NSP antigens. The authors say this suggests that antibodies against ORF7a, ORF8, and NSP antigens are either short-lived or are only generated in response to more severe infection.
The team also found that the anti-N response preceded the anti-spike response and was consistently greater across all time points. Furthermore, levels of anti-N protein and anti-spike immunoglobulin G titers were strongly correlated in both acutely infected and convalescent individuals.
The team says this indicates that people who mounted a robust antibody response against SARS-CoV-2 tended to have a robust response against both antigens.
The researchers also found that levels of antibody titers against the spike and N protein were significantly higher than those against ORF7a and ORF8.
“Together, these data reveal the antibody response against SARS-CoV-2 is largely driven against the spike and N protein and that the anti-N protein antibody response precedes the response against the spike,” says the team.
Variability in response among acutely infected individuals
To understand variability in humoral response between the acutely infected participants, the researchers clustered the subjects into “high,” mid,” and “low” responder groups based on their antibody titers against spike, the N protein, ORF7a, and ORF8.
Those in the high responder cluster were further from symptom onset at the time of plasma sampling and were therefore hospitalized for longer than those in the mid and low responder groups. No statistical difference in age or sex between the three groups was observed.
More than one-quarter of participants in the high responder group scored higher on a measure of pneumonia severity, suggesting more severe infection among this group.
Individuals in the high and mid responder groups had robust antibody responses against the spike protein. Still, the high responders had a larger response to N protein than mid responders did. Furthermore, high and mid responders were more likely to mount antibody responses against ORF8 and NSP. The low responders generally did not have antibody responses against any of the antigens tested.
“Our data reveal that acutely infected subjects who were hospitalized for a longer duration mounted a larger antibody response against N protein and were more likely to mount a response against other SARS-CoV-2 antigens,” say the researchers.
Variability among convalescent individuals
The team also clustered convalescent individuals into three groups based on their antibody responses against the spike and N protein.
To test associations between infection severity and antibody responses within this group, participants were scored based on the severity and duration of self-reported symptoms and whether hospitalization was required.
Notably, more than half of those in the high responder group had severe infection, suggesting that infection severity is linked to higher antibody titers.
Convalescent high responders had higher titers against not only the N protein but also against spike and ORF8, compared with mid and low responders.
“In combination with the acutely infected cohort, our data reveal subjects with more severe infection are mounting a larger antibody response at both acute and convalescent time points,” says the team.
Testing the Memory B cell response
Next, the researchers tested the memory B cell (MBC) response to SARS-CoV-2 infection using peripheral blood mononuclear cells (PBMCs) isolated from convalescent subjects.
Notably, MBCs mainly targeted spike, rather than N protein or ORF8, and high responders had larger MBC responses against spike than mid and low responders, with the titer of anti-spike antibodies correlating with the magnitude of the anti-spike MBC response.
The team says the findings show that the MBC response is mostly directed against the spike protein and that high responders mount both a larger antibody and MBC response following SARS-CoV-2 infection.
“Together, this study reveals that subjects with a more severe SARS-CoV-2 infection exhibit a greater overall antibody response to the spike and nucleocapsid protein and a larger memory B cell response against the spike,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Wilson P, et al. SARS-CoV-2 infection severity is linked to superior humoral immunity against the spike. bioRxiv, 2020. doi: https://doi.org/10.1101/2020.09.12.294066
- Peer reviewed and published scientific report.
Guthmiller, Jenna J., Olivia Stovicek, Jiaolong Wang, Siriruk Changrob, Lei Li, Peter Halfmann, Nai-Ying Zheng, et al. 2021. “SARS-CoV-2 Infection Severity Is Linked to Superior Humoral Immunity against the Spike.” Edited by Stacey Schultz-Cherry. MBio 12 (1). https://doi.org/10.1128/mbio.02940-20. https://journals.asm.org/doi/10.1128/mBio.02940-20.