Exposing a high titer of surface-dried SARS-CoV-2 to a low dose of UV-C light for just a short time completely reduced the infectivity of the virus.
The application of UV-C light is already an established technique for decontaminating surfaces and has already proven effective against other viruses and bacteria.
It has also recently been shown that SARS-CoV-2 is sensitive to inactivation using this technique. However, the exposure times needed for complete inactivation of the virus were not conducive with the UV-based methods used in large-scale decontamination processes.
Now, Michael Schindler and colleagues have shown that surface-dried SARS-CoV-2 can be inactivated by low-dose UV-C light in a “real-life” setting in as little as 2 seconds using a handheld device.
“UV-C irradiation is a rapid and cost-effective technology to decontaminate surfaces from high-titer SARS-CoV-2,” says the team.
A pre-print version of the paper is accessible on the server bioRxiv*, while the article undergoes peer review.
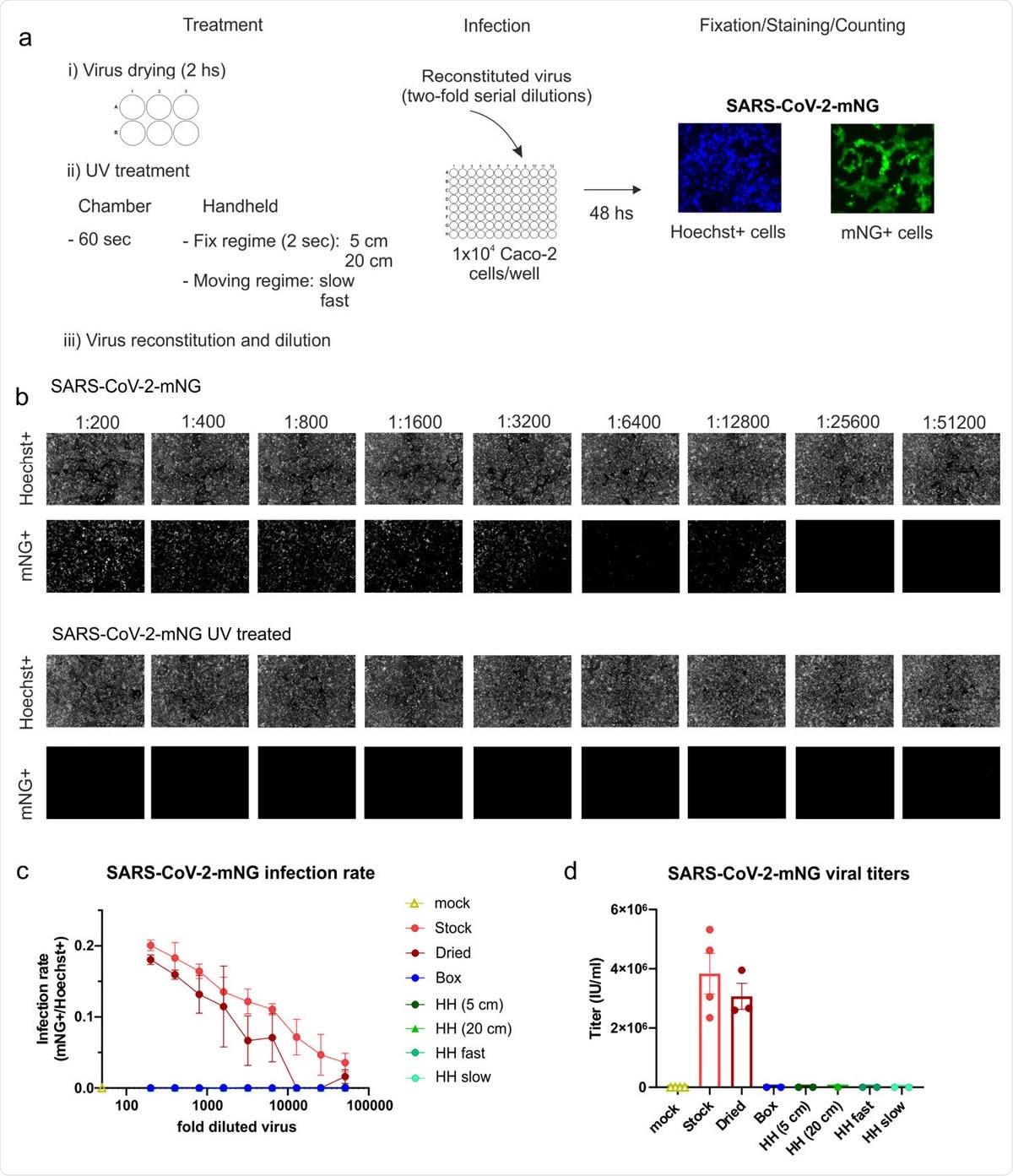
Inactivation of SARS-CoV-2 by UV-C light treatment. (a) Experimental layout of the different UV-treatments and the infection assay employed using the green-fluorescent virus SARS-CoV-2.mNG. (b) Primary data showing the results of the infection assay using the non-treated stock virus as a positive control and the UV-treated virus (HH, fast-moving regime). In the upper row, the total amount of cells for each well of the two-fold serial dilution of virus is shown as Hoechst+. In the 249 lower, infected cells are visualized indicated as mNG+ cells. (c) Infection rate curves for UV-irradiated SARS-CoV-2-mNG using different UV251 treatments. The graph shows the infection rate at each two-fold serial dilution, calculated as the number of infected cells (mNG+) over the total number of cells (Hoechst+) for the non253 treated viral stock (n=4), dried viral stock (n=3), and dried and UV-irradiated virus using five different UV-treatments (n=2). Data are presented as mean +/- SEM of the number of biological replicates indicated above. (d) SARS-CoV-2-mNG viral titers after UV-treatment. The graph shows the viral titers calculated in IU/mL for the mock-infected, non-treated, and dried stock as well as the dried and UV-irradiated virus under the different treatments. The number of biological replicates is directly plotted and indicated in 1c. Data are presented as mean +/- SEM.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Rapid, efficient, non-chemical decontamination procedures are urgently needed
As the COVID-19 pandemic continues to sweep the globe, there is an urgent need for rapid, efficient, non-chemical procedures to decontaminate surfaces of the causative agent SARS-CoV-2.
Application of UV-C irradiation is a well-established, safe procedure used for the environmental control of pathogens and has already proved effective at inactivating SARS-CoV-1 as well as other coronaviruses.
Recently, the sensitivity of SARS CoV-2 to inactivation by UV-C irradiation has also been demonstrated.
However, the doses and exposure times needed to inactivate SARS-CoV-2 completely have been in a range that precludes efficient application of UV-based methods for use in large-scale decontamination of surfaces, say Schindler and colleagues.
“One critical question is the suitability of this technology in a ‘real-life’ setting in which the exposure time of surfaces or aerosols should be kept as short as possible to allow for a realistic application, for example, in rooms that need to be used frequently as operating rooms or lecture halls,” writes the team.
What did the researchers do?
Simulating a situation where exhaled droplets or aerosols from infected individuals contaminate surfaces, the team generated a high-titer stock of infectious SARS-CoV-2 and spotted 35uL of this stock (in triplicates) in 6-well plates which were dried for two hours at room temperature.
The plates were then either left untreated or were exposed to five UV-C regimens.
These regimens included inactivation for 60 seconds in a UV-C box designed to disinfect medium-size objects; 2-second UV-C exposure at a distance of either 5 or 20 cm using a handheld disinfection device and, finally, a movement regimen simulating decontamination of surfaces using the handheld UV-C device.
For the latter, the device was moved at a “slow” speed (about 3.75cm per second) and “fast” speed (about 12cm per second) at a distance of 20 cm from the plates.
The UV-C exposure in the box for 60 seconds corresponded to an irradiation dose of 800 mJ/cm²; the 2-second exposure at 5 cm with the handheld device corresponded to 80 mJ/cm² and 2-second exposure at 20 cm corresponds to 16 mJ/cm².
For the “slow” and “fast” moving regimens, the team calculated UV-C irradiation doses of 2.13 mJ/cm² and 0.66 mJ/cm², respectively.
All five UV-C regimens, but not drying, were effective
Drying for two hours did not have any significant impact on SARS-CoV-2 infectivity, suggesting that exhaled virus present in droplets or aerosols retains infectivity on surfaces for at least two hours.
Treatment with UV-C, on the other hand, effectively inactivated the virus under all five exposure regimens.
Strikingly, even the short exposure to an irradiation dose of 0.66 mJ/cm in the fast-moving regimen resulted in a complete reduction of SARS-CoV-2 infectivity.
An easy, rapid, chemical-free decontamination method
The team says the findings show that that SARS-CoV-2 is rapidly inactivated by relatively low doses of UV-C irradiation.
“Altogether, we establish the effectiveness of UV-C treatment against SARS-CoV-2 in a setting designed to simulate realistic conditions of decontamination,” write the researchers.
“The easy, rapid, chemical-free, and high efficacy of UV-C treatment to inactivate SARS-CoV-2 demonstrates the applicability of this technology in a broad range of possible settings,” they conclude.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources