The coronavirus disease (COVID-19) pandemic has infected over 35 million people worldwide and caused more than 1 million deaths so far, making it clear that it is an urgent threat to public health worldwide. While COVID-19 can cause mild disease in many people, with only cough and fever as reported symptoms, studies show that up to 30% of those infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may require hospitalization, and some patients will need intensive clinical intervention for acute respiratory distress syndrome.
Across the globe, public health responses have been focused on limiting new infections by preventing community transmission through social distancing, usage of masks, shutting down non-essential services, and enforcing travel restrictions. These interventions have had devastating social and economic impacts, along with a steep increase in reported mental health issues.
At a time when nations are experiencing increased pressure to re-open economies and return to normal life, there is an urgent requirement for tests that can predict which individuals are at higher risk of severe COVID-19 leading to hospitalization. A risk prediction test will enable workplaces to identify at-risk employees and make them avoid taking up client-facing roles or work from home. In the healthcare setting, a good risk prediction test could guide patient triage when resources become limited and also can help prioritize tests and vaccination, whenever one becomes available. On an individual level, knowledge of personal risk can help individuals make informed choices about their day-to-day activities.
While determining the risk of severe COVID-19, age, and gender are usually the only considerations. A recent preprint paper published in medRxiv,* discusses how researchers from Genetic Technologies Limited, Australia, used the UK Biobank data to develop a comprehensive model that can predict severe COVID-19 risk by incorporating comorbidity risk factors, demographic information, and a set of genetic markers.
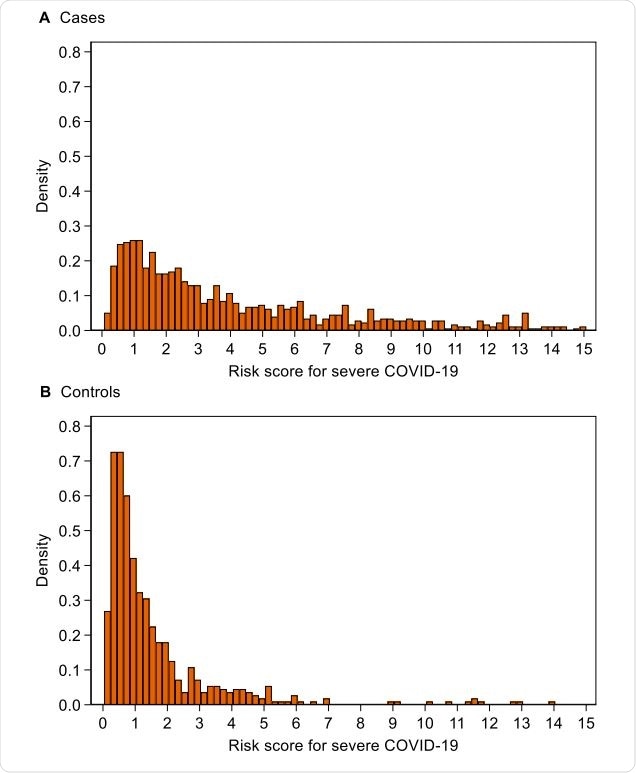
Distribution of risk score for severe COVID-19 risk score for (A) cases and (B) controls. Note that 130 (13%) cases and 6 (1%) controls with scores of 15 or over have been omitted to facilitate the display of the distribution

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Impact of age and gender were diminished by the other risk factors
Using previously published data, the team was able to identify clinical risk factors and a set of 64 single-nucleotide polymorphisms (SNPs). They studied 1,582 UK Biobank participants aged 50 years or above who tested positive for SARS-CoV-2. By using logistic regression, the team devised a genetic model for severe COVID-19 risk in these patients. Out of the 1,582 patients, 1,018 had severe COVID-19, while the remaining 564 participants did not experience severe disease.
The model the team developed incorporating the SNP score and other clinical risk factors proved to have 111% better discrimination of disease severity compared to a model that took into account only age and gender. The impact of age and gender was diminished by the other risk factors, suggesting that it is the other factors, and not age and gender, that advise the risk of severe disease. In the entire UK Biobank data, most patients were at low or just slightly elevated risk, but 1/3rd of them were at 2-fold or more increased risk.
Relying only on age and gender will ignore the risk in younger people with comorbidities
Based on the results of the study, the authors developed a model that facilitates accurate prediction of severe COVID-19 risk. They believe that relying only on age and gender to determine the risk of severe disease will unnecessarily classify older but healthy people as high-risk individuals and will fail to accurately measure the increased risk some younger people with comorbidities run to develop severe COVID-19.
The team does agree that their study has some limitations like using the source of test results as a proxy for disease severity, which renders a good chance misclassification of disease severity. Also, BMI and smoking status were taken from the baseline assessment data and hence may not represent the current status of the participants, which may have made the variables statistically insignificant.
Moreover, as COVID-19 testing in the UK was limited to people with recognizable symptoms, essential workers, contacts of known cases, or people with travel history until mid-May, the Biobank dataset may not include many asymptomatic or mild cases from the first wave. Despite this, the authors believe their results are applicable to patients with severe COVID-19 requiring hospital care.
“Our risk prediction test for severe COVID-19 in people aged 50 years or older has great potential for wide-reaching benefits in managing the risk for essential workers, in healthcare settings and in workplaces that seek to re-open safely.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources