Serological antibody immunoassays are one of the essential tools to combat severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. In a new study, Immunoglobulin G (IgG) antibodies are detected in a large cohort, lasting up to 140 days. The researchers propose an alternative to reverse transcription-polymerase chain reaction (RT-PCR) positive status as a standard for assessing SARS-CoV-2 antibody assays and show robust performance metrics for the AbC-19 rapid test.
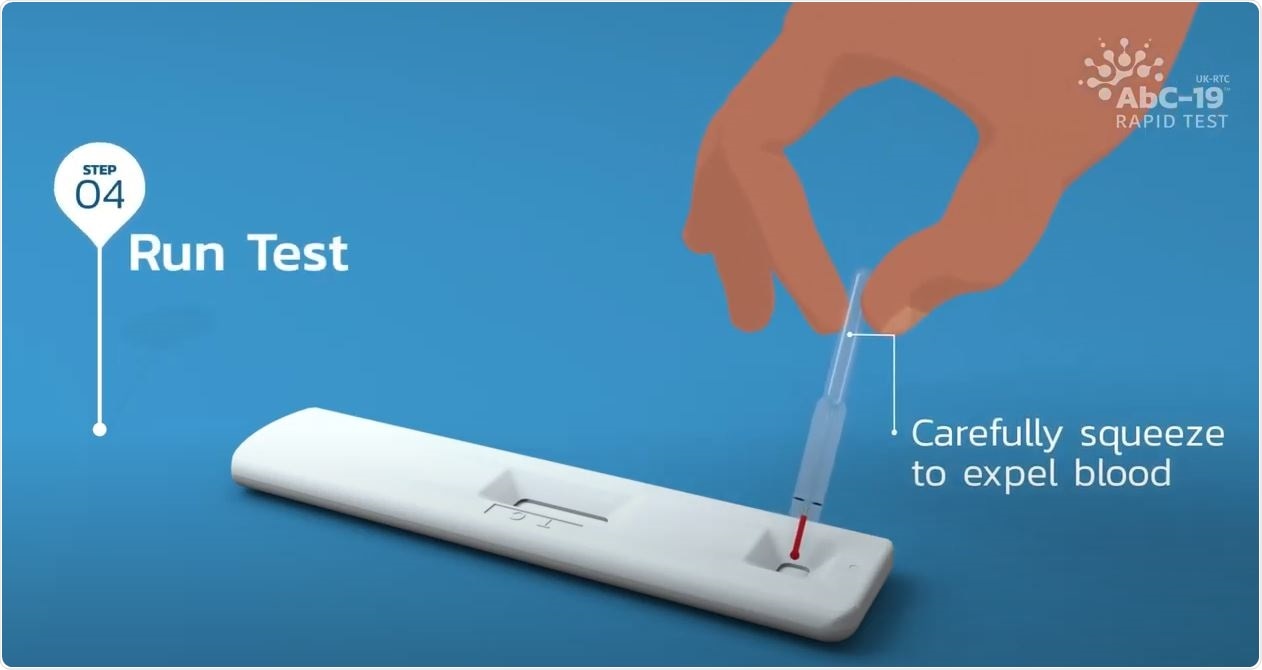
Image Credit: Abingdon Health

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The COVID-19 (coronavirus disease 2019), caused by SARS-COV-2 the virus, has caused over 1 million deaths from over 35 million confirmed cases of infection globally over a short period (10 months). While the SARS-CoV-2 pandemic has necessitated rapid translation of knowledge from lab to clinic, an unprecedented interest has gained in serological immunoassays to detect antibodies to this novel virus. The dynamics of the immune response to SARS-CoV-2 is not yet clearly understood. It is essential to detect SARS-CoV-2 specific antibodies accurately. This is essential for building biobanks of convalescent sera for treatment, monitoring immune response to infection, and assessing responses to vaccination programs.
In their recent medRxiv* paper, Louise J Robertson et al. report the persistence of SARS-CoV-2 IgG up to 140 days (20 weeks) post-infection, across three antibody immunoassays and propose a standard for assessing SARS-CoV-2 antibody assays. The authors use a ‘pseudo gold standard’ cohort (n=348 positive, n=510 negative) to determine the sensitivity and specificity of the three commercial immunoassays (EuroImmun; Sens. 98.9% [97.7-99.7%]; Spec. 99.2% [98.4-99.8%]; Roche; Sens. 99.4% [98.6-100%]; Spec. (96.7% [95.1-98.2%]; Abbott; Sens. 86.8% [83.1-90.2%]; Spec. (99.2% [98.4-99.8%]). The UK-RTC AbC-19 lateral flow immunoassay shows a sensitivity of 97.70% (95.72%-99.34%) and specificity of 100% (100.00-100.00%). The study cohort included 880 people in Northern Ireland.
There is no clear gold standard for reference to assess SARS-CoV-2 immunoassays. RT-PCR is used as a reference standard; however, it is limited by a short temporal window for a positive diagnosis and exhibits potential for false-negative results. With lockdown measures and “flattening the curve” strategies, many cases were largely unconfirmed or undetected. The commercial serology immunoassays are laboratory-based and measure IgG antibody levels in plasma or serum. Alternatively, lateral flow immunoassays (LFIAs), requiring a finger-prick blood sample, can be used at home or POC (point-of-care).
Currently, in the UK, a limited number of laboratory-based chemiluminescence immunoassays are approved, including the Roche Elecsys AntiSARS-CoV-2 IgG/IgA/IgM against the SARS-CoV-2 Nucleocapsid antigenic region (Roche Diagnostics, Basel, Switzerland) and the Abbott SARS-CoV-2 IgG assay against the same antigenic region (Abbott Diagnostics, Abbott Park, IL, USA).
The authors use these tests to detect antibodies generated against the S1 domain of the spike antigenic protein of SARS-CoV-2, to characterize a large number (880) of pre-pandemic and pandemic COVID-19 blood samples from within Northern Ireland. IgG antibodies to both the spike protein and nucleocapsid protein are persistent even after 140 days after RT PCR positive status; the authors report a statistically significant decline over time, but the levels remain detectable at 140 days.
The authors call for further studies on large cohorts with sequential antibody immunoassays performed on symptomatic and non-symptomatic individuals as well as those with mild and severe COVID-19.
To assess sensitivity and specificity, they developed a ‘pseudo-gold-standard’ against which to analyze assays, which does not rely on a single test as reference. They report performance metrics for the UK-RTC AbC-19 rapid lateral flow immunoassay (LFIA) against a characterized panel of 304 positives established using the ‘pseudo gold standard’ system and 350 negative samples.
Their results show a strong correlation between all three immunoassays, with shortcomings in the Abbott system, suggesting an overestimated positive cut-off. Furthermore, they also present results of independent validation of the UK-RTC AbC-19 POC LFIA against a cohort of 304 known positives according to this ‘pseudo-gold-standard’ system and 350 known negative samples for IgG to SARS-CoV-2.
It is crucial to consider the prevalence when interpreting an assays’ sensitivity and specificity in a low prevalence scenario. Even slightly lowered performance metrics can result in large numbers of false-negative and false-positive results. The authors observe the high sensitivity of the AbC-19 LFIA - in which case, false-positives are unlikely, though false negatives may occur. This will underestimate true prevalence in a study.
For individuals, it may cause anxiety. However, a positive antibody test will help arrest infection spread.
In conclusion, the researchers report the longevity of antibodies against the SARS-CoV-2 virus in the plasma of a large cohort of individuals - lasting up to 140 days; and they have developed a ‘pseudo gold standard’ reference cohort against which to assess immunoassay performance.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
SARS-CoV-2 antibody testing in a UK population: detectable IgG for up to 20 weeks post infection. Louise J Robertson, Julie S Moore, Kevin Blighe, Kok Yew Ng, Nigel Quinn, Fergal Jennings, Gary Warnock, Peter Sharpe, Mark Clarke, Kathryn Maguire, Sharon Rainey, Ruth Price, William Burns, Amanda Kowalczyk, Agnes Awuah, Sara McNamee, Gayle Wallace, Steve Sager, Connie Chao Shern, M. Andrew Nesbit, James McLaughlin, Tara Moore, medRxiv 2020.09.29.20201509; doi: https://doi.org/10.1101/2020.09.29.20201509
- Peer reviewed and published scientific report.
Robertson, Louise J., Julie S. Moore, Kevin Blighe, Kok Yew Ng, Nigel Quinn, Fergal Jennings, Gary Warnock, et al. 2021. “Evaluation of the IgG Antibody Response to SARS CoV-2 Infection and Performance of a Lateral Flow Immunoassay: Cross-Sectional and Longitudinal Analysis over 11 Months.” BMJ Open 11 (6): e048142. https://doi.org/10.1136/bmjopen-2020-048142. https://bmjopen.bmj.com/content/11/6/e048142.