In anticipation of coronavirus disease (COVID-19) vaccine deployment, the Australian and US researchers utilized an age-structured mathematical model to appraise the potential benefits of optimizing age-specific dose allocation for suppressing SARS-CoV-2 transmission – and reaffirmed the notion that vaccination alone may be inadequate to achieve herd immunity in some settings. The study is currently available on the medRxiv* preprint server.
Both safe and sufficiently effective vaccine is needed to fully curtail the pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), as the virus is highly transmissible and notoriously onerous to contain.
However, initial vaccine deployments should be targeted not only at those at the most significant risk of infection and disease development but also those most responsible for the ongoing transmission. In other words, targeting age groups that contribute more to the transmission of infection may dramatically enhance the effectiveness of COVID-19 vaccination.
Current estimates for SARS-CoV-2 herd immunity thresholds are between 60 and 70%, which corresponds to approximately 90% population-wide vaccination coverage if we have a vaccine that is at least 70% effective. However, if we incorporate population heterogeneity, these thresholds may be considerably lower.
This results from young-to-middle-age groups having high contact rates, combined with high infectiousness and susceptibility to infection. Eliminating these persons from the susceptible pool would, in turn, result in disproportionate effects on the transmission potential.
Such observations are central for vaccination strategies, as they imply that the age-specific characteristics of both social mixing and SARS-CoV-2 infection may be leveraged to augment the efficiency of future vaccine campaigns.
This is why a research group, led by Dr. Michael T. Meehan from the Australian Institute of Tropical Health and Medicine at James Cook University in Townsville, Australia, recently developed a mathematical model that optimized age-specific dose allocation and provided the global distribution of minimum vaccination coverage necessary for achieving herd immunity. Dr. Meehan was supported by researchers at the Australian National University, Monash University and the University of Hawaiʻi at Mānoa.
Modeling vaccine coverage levels
In order to estimate age-specific transmission rates among infected individuals in 179 countries, this study employed an age-stratified SARS-CoV-2 transmission model that assimilates age-dependent susceptibility and disease severity calibrated to COVID-19 patient data.
The researchers then used the candidate vaccine profiles developed by the World Health Organization to select optimization targets designed to reduce transmission, defined through the reduction in the effective reproduction number or Reff. Investigating such a range of alternatives also accounted for parameter uncertainty.
Two separate modes of action for vaccine candidates were considered: those that reduce the recipient's sensitivity to infection, and those that safeguard against symptomatic disease development in individuals who become infected with SARS-CoV-2.
Moreover, the costs and feasibility of age-specific vaccine roll-out were not factored in to avoid excessive speculation. Nonetheless, besides the optimal global solutions identified for each age group/setting, the researchers have also specified a range of possible age-specific coverage levels with near-equivalent (within 1%) transmission reduction potential that may be chosen if proven more cost-effective.
Tailored age-specific vaccination strategies
Across 179 countries included in this study, the researchers have found that the highest priority individuals belong to those between 30 and 59 years of age, primarily due to their high contact rates and a higher risk of infection and disease.
"Whether the goal is to minimize transmission for a fixed number of doses or to minimize the number of doses required to achieve a certain reduction in transmission, our analysis indicates that dosage requirements or transmission rates can be halved under tailored age-specific vaccination strategies", further explain study authors.
In any case, this paper shows that a vaccine with less than 100% efficacy may need substantial population-level coverage to achieve herd immunity, albeit this threshold can be substantially reduced via targeted vaccination – as suggested by certain studies that account for heterogeneities in population sensitivity and mixing.
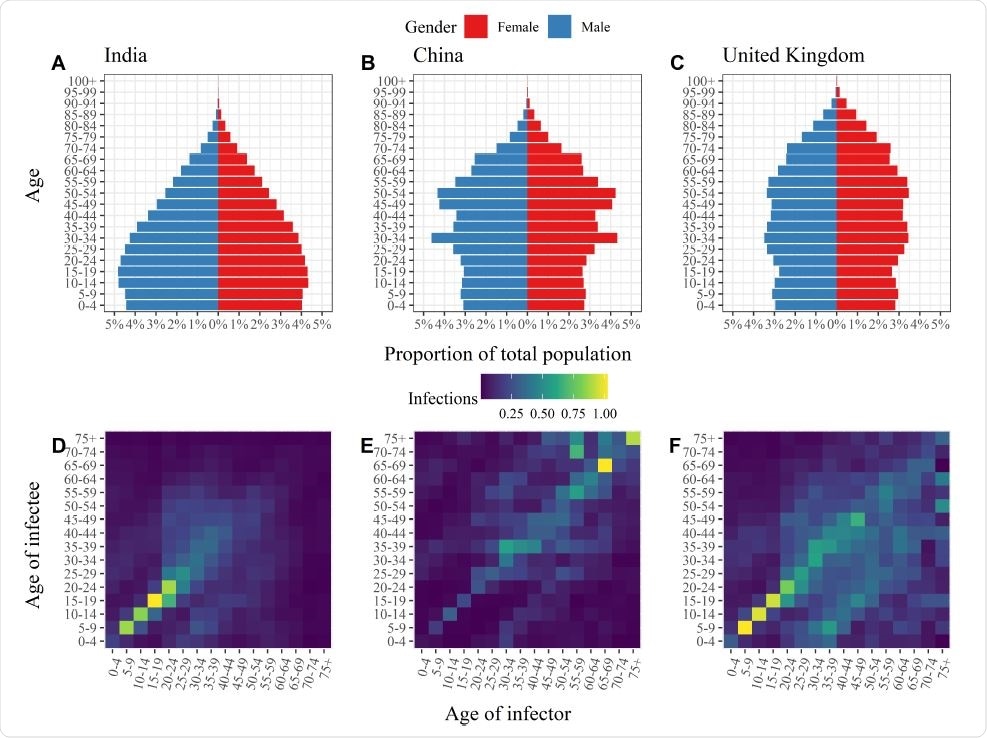
Age distributions and age-specific transmission rates. Population pyramids (Panels A-C) and transmission matrices (Panels D-F) for India (left), China (middle) and the United Kingdom (right). In Panels D-F the colouring of the ith row and jth column of the transmission matrices represents the average number of infections in age group i generated by an individual in age group j over the course of an infectious episode with COVID-19. The elements of each matrix have been rescaled such that the maximal eigenvalues of the respective transmission matrices match the basic reproduction numbers (R0) estimated by Abbott et al.15, namely India: 2.2; China: 2.6; and the United Kingdom: 2.3.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Practical implications
If and when we see an approved COVID-19 vaccine with worldwide availability, a pivotal step will be to allocate the doses in a manner that curtails viral transmission most efficiently, since initial supplies will unquestionably be limited.
"Our study shows that setting- and age-specific optimization of vaccine allocation can provide substantial improvements in efficiency over uniform vaccination programs, saving up to half of the available doses to achieve the same reduction in transmission in some settings", emphasize study authors in this medRxiv paper.
Furthermore, this analysis has also highlighted the often overlooked and unappealing outcome that vaccination alone may not be enough to entirely suppress COVID-19 – especially if the vaccine fails to stop the initial infection.
Subsequently, the authors state that this may open the door for permanent control measures alongside vaccination protocol, which may include social distancing or improved hygiene. But for now, we can just wait and observe how the first vaccines that come to the market will behave in the real-world setting.
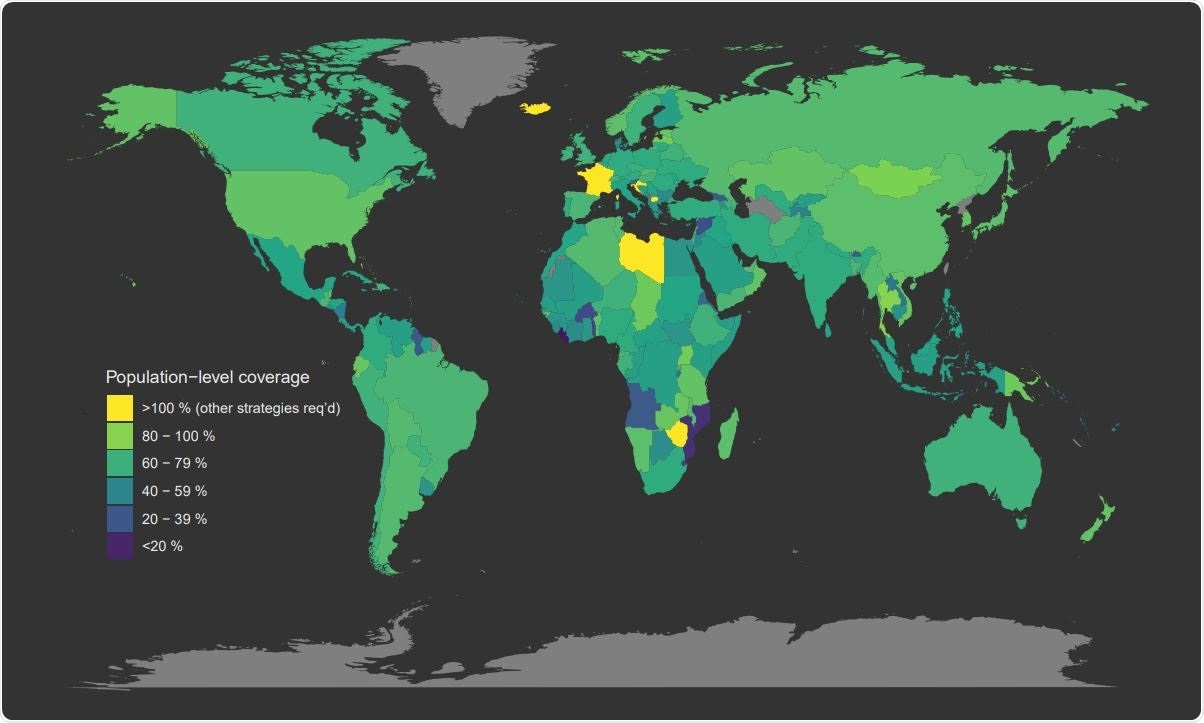
Global target vaccination coverage under uniform vaccination policy. Map of the minimum target vaccination coverage required to achieve herd immunity under uniform vaccine allocation programs. Countries coloured bright yellow are incapable of achieving herd immunity through vaccination alone (i.e., their minimum coverage thresholds exceed 100%).

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.