Three coronaviruses (CoVs) have caused global outbreaks within the past 20 years, and with the COVID19 pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) still ongoing, methods that can rapidly inactivate these viruses can play critical roles in ensuring public safety and safeguarding personal health.
Prior Methods of Inactivation
The primary spread of SARS-CoV-2 is by respiratory droplets and aerosols, or contact with contaminated surfaces. While droplets travel short-range, aerosols can carry the virus long-range. If these deposit on surfaces, the latter become infectious. Thus, the environment must be sanitized and viruses inactivated in order to control viral spread.
As of now, chemical agents, ultraviolet irradiation, and heat treatment have all been used, but the latter is the most attractive because of the short time required for treatment and the simplicity of application. Coronaviruses are enveloped viruses with a lipid bilayer envelope from which spikes project.
Both the envelope and the spike protein are denatured by heating for more than one minute to 56oC or more, reducing viral titers by 6 log10 or more. At a temperature of 56-65 oC, inactivation occurred by heating for 15-60 minutes, but by raising the temperature to 70-100 oC, only 1-15 minutes was sufficient to reduce the viral titer by 4.5 log 10. At still higher temperatures (92 oC), a 6 log10 reduction was achieved by heat treatment at 15 minutes.
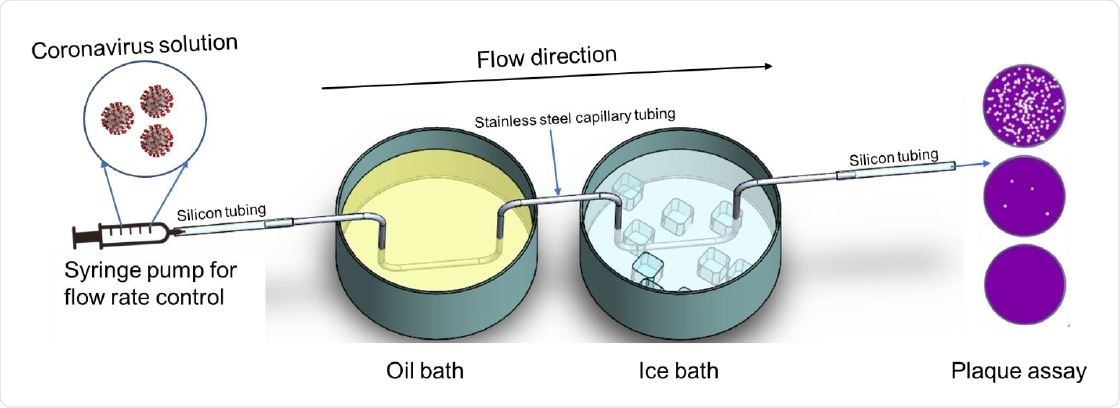
Schematic illustration of the virus heat inactivation system

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Providing Proof of Concept for Rapid Heat Inactivation
The researchers developed a simple method to expose viruses to extreme heat for very brief periods. This system can be retrofitted into various living spaces and existing heating, ventilation, and sewer systems to ensure human safety. This can be adapted to disinfect liquids or airborne viruses and to design instruments to accomplish this. This method can also be used to evaluate the sensitivity of other viruses to heat and to develop a broad-based approach to sub-second inactivation of viruses by heat.
The current study aims to reduce the time still further, to less than a minute, so that viral particles in air or liquids can be quickly and efficiently inactivated in many everyday settings. Beyond this, keeping liquids at high temperatures is not feasible for more extended periods, while air must be treated almost instantly.
The researchers used a simple flow-through heating and cooling method, with the aid of a stainless steel capillary tube. This allowed them to examine the effect of heating coronaviruses to heat for just 0.1 to 1 second over a temperature of 35-100 oC. The findings will be important for not just coronaviruses but also other viruses like dengue virus, influenza virus, and measles virus, all of which are lipid enveloped with envelope proteins.
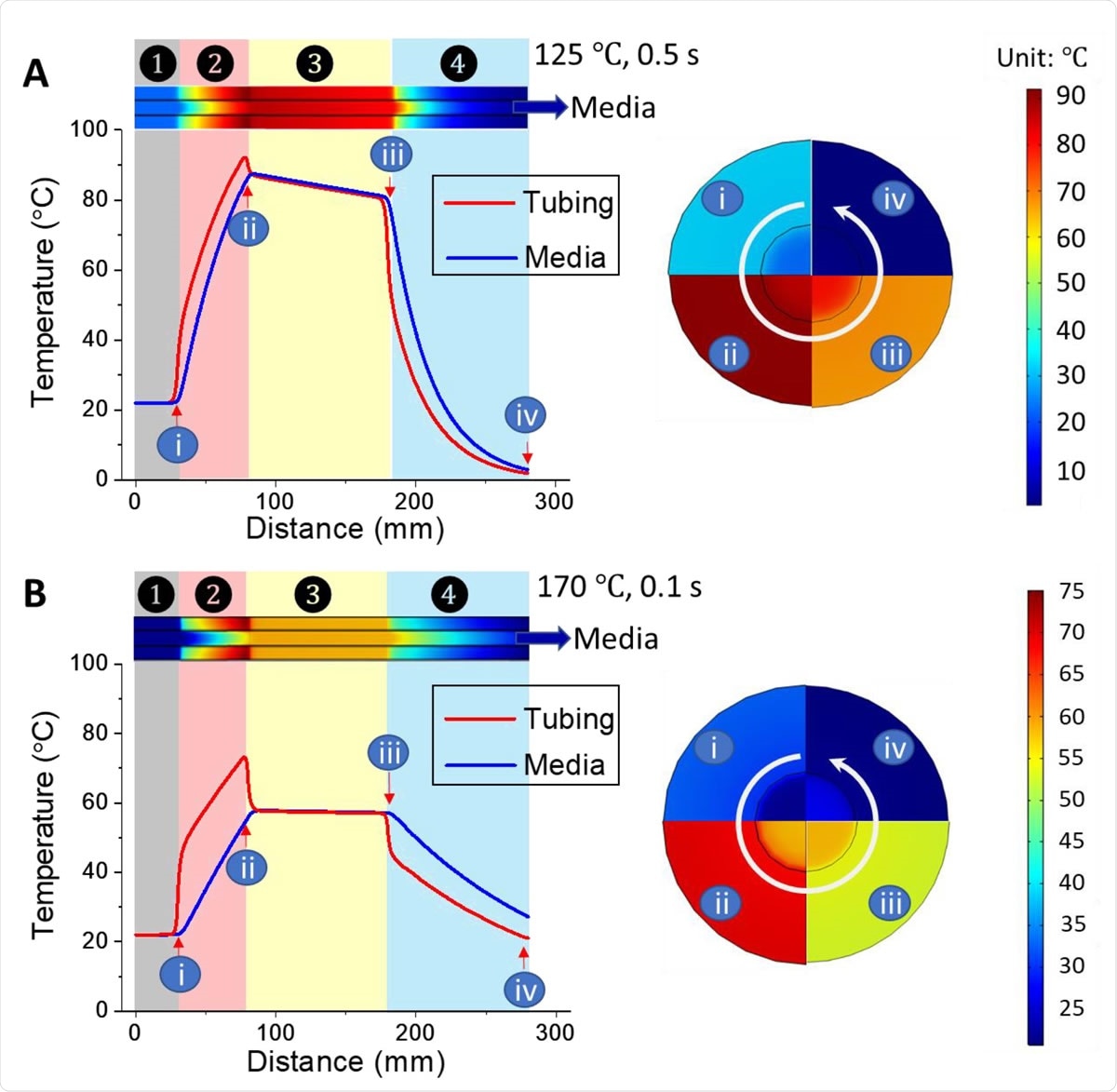
The simulated temperature distribution of the entire heat inactivation system when using oil bath to apply and sectional views of positions i - iv are displayed in the right circle: (A) 125 ℃, 0.5 s exposure, and (B) 170 ℃, 0.1 s exposure. Zone ○1 pre-oil bath; Zone ○2 oil bath; Zone ○3 ambient air; Zone ○4 Ice bath.
Accurate Temperature Assessment
The researchers first found a way to accurately measure the instantaneous temperature of the solution containing the viruses during heating by using a thermocouple at the junction of the SS tube. With slower flow, a slight drop in measures temperature occurs, which is corrected by calibrating the curves accordingly.
COMSOL Simulation
The researchers then simulated the heat transfer from the SS tube to the solution containing the coronavirus flowing within the tubing, using the COMSOL MultiphysicsTM program. The temperature is found to go up rapidly in the oil bath zone, reduce slowly in the air zone, and drop rapidly in the ice bath. The effective heat treatment region was designated from the highest temperature reached after the oil bath and just before the ice bath, about 9.5 cm long. The simulated exposure time of the solution to be disinfected was about two times the set time of ~1 second when the applied exposure time was set to 0.5 cm. The simulation was repeated using a higher temperature and a faster flow.
Heat inactivation of MHV 256
Coronaviruses are relatively heat-stable at room temperatures, and only above 65 oC does viral inactivation begin to occur. At this point, temperature-sensitive viral destruction is apparent with even small rises in applied temperature, causing a substaintial increase in the death rate.
The viral load of SARS-CoV-2 is 7 × 106 per mL on average. To test the capacity of the system to achieve rapid heat inactivation, the researchers used sub-second exposure and found a 6 log 10 or more reduction in viral titer with the oil bath temperature at 115 oC with 1 second residence time.
To achieve the same with a lower exposure time of 0.5 second, the temperature must be raised to 125 oC or more, while if the time is further reduced to 0.25 seconds, the reduction in viral titer is 5 log10. At 0.1 second efficient inactivation is not achieved even at 170 oC.
Using the residual infectivity, a re-plot showed that the inactivation of the virus required 0.25 seconds at least at an exposure temperature of 85.2 oC. The fastest heat treatment for complete viral inactivation requires 0.5 seconds, with the actual temperature to which the virus is exposed being 83.4 oC.
Implications
The researchers conclude, “This is the first experimental result that shows that sub-second exposure to high 300 temperature is sufficient to inactive the infectibility of CoV. Our study fills the gap of sub-second heat treatment under applied actual temperature.”
By providing essential data on heat inactivation, the researchers have paved the way for developing a quick, cheap, and efficient approach for coronavirus inactivation in real-world settings.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources