Researchers have found that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can infect the brain cells, mainly the astrocytes, and negatively affects cognition and neuronal cells.
The SARS-CoV-2 virus sweeping across the globe mostly affects the human respiratory system. However, on one end, people infected with the virus show no symptoms (asymptomatic), while at the other extreme, patients have severe respiratory problems leading to death.
Several studies have now reported that the virus can also affect other organs. About 30% of patients show neurological or neuropsychiatric symptoms. More than half continue showing these symptoms even after three months, with significant damage to the nervous system.
To understand how SARS-CoV-2 affects the brain, researchers recruited 81 patients infected with the virus and presenting with mild symptoms that required no hospitalization. Their work is published on the preprint server medRxiv* in October 2020.
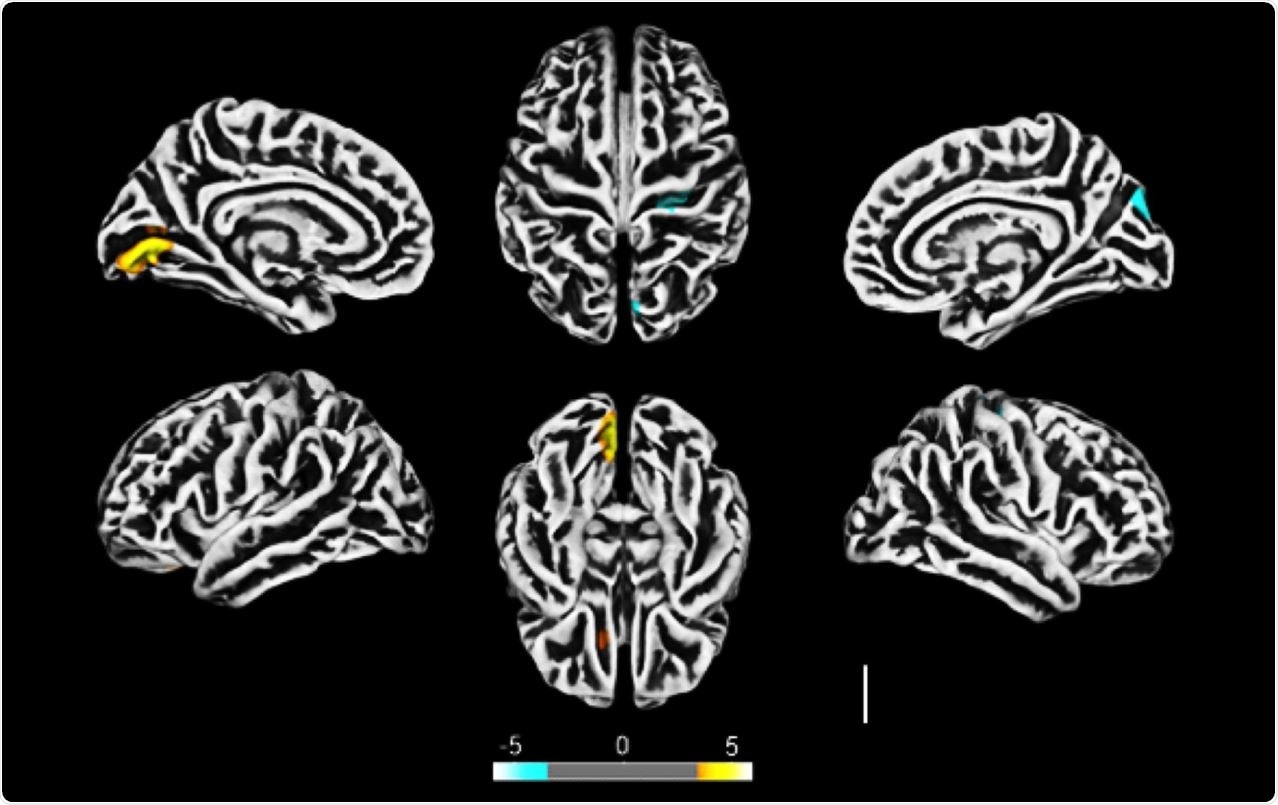
Altered cerebral cortical thickness is associated with neuropsychiatric symptoms in COVID-19 patients. a) Surface-based morphometry using high-resolution 3T MRI. Yellow represents areas of decreased cortical thickness: left lingual gyrus, calcarine sulcus (and cuneus), and olfactory sulcus (and rectus gyrus) . Blue represents areas of increased cortical thickness: central sulcus (precentral and postcentral gyrus) and superior occipital gyrus. Representative image of the analysis of 81 subjects tested positive for SARS-CoV-2 who had mild respiratory symptoms and did not require hospitalization or oxygen support compared to 145 healthy volunteers (without diagnosis of COVID-19) . The analysis was performed within a median interval of 54 days. b) Correlation between BAI performance and right orbital gyrus thickness. The data depicts Pearson’s correlation coefficient . c) Correlation between TRAIL B performance and right gyrus rectus thickness. Data depict Pearson’s correlation coefficient and region of interest in representative images.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
SARS-CoV-2 virus found in brains of patients
All the recruited patients underwent MRI scanning of the brain. The team saw reduced cortical thickness in some areas of the brain and increased thickness in other parts.
Sixty-one patients also underwent a neuropsychological interview, which evaluated them for anxiety and depression, 21 to 120 days after their COVID-19 diagnosis. Also, the authors also tested their memory and cognitive functions.
About 28% of the patients showed signs of anxiety, and 20% showed signs of depression. About 28% of the patients also showed abnormal logical memory performance.
Upon correlating the cortical thickness changes to the neuropsychological evaluation, the team found that the thinner cortex affected verbal memory, suggesting COVID-19 can affect brain structure and result in changed brain functions.
The change in brain functions could be because of inflammatory changes secondary to the infection or could be because of the ability of the virus to invade the central nervous system (CNS).
To probe further, the team also collected brain tissue samples from 26 patients who had succumbed to COVID-19. They found five individuals had changes in the brain that could arise because of inflammation. The viral genetic material and spike protein was found in all of these samples, in about one-third of the cells.
The spike protein was found mainly in the astrocytes, cells that perform several functions in the CNS, and in the neurons.
Upon analyzing the infected astrocytes further, the researchers found 233 proteins expressed in the cells. These proteins are involved in several biological processes, such as carbon metabolism, glycolysis, and biosynthesis of amino acids. Thus, the infection could lead to increased metabolic activity and decreased metabolites used to support neuronal metabolism.
Brain infection could impair cognition and neurons
Next, the authors investigated if the infection in astrocytes could affect neurons. They cultured SH-SY5Y neurons in a medium with SARS-CoV-2 infected astrocytes.
They found that the infected astrocytes induced apoptosis in the neurons, indicating that the virus infection could trigger events that could kill neurons.
Studies on how the SARS-CoV-2 infection affects the brain have raised questions on whether this is because of secondary affects of the infection or if the virus can invade the CNS.
The authors write their results indicate this is because the virus can invade the CNS. Other studies have also found viral particles in the brain, localized in the microcapillaries, and in neurons.
Furthermore, the infection of the astrocytes could affect neurons, as astrocytes metabolism is essential for neural function. In the astrocyte-infected cells, the authors found a decrease in the intermediates of glutamine metabolism. Glutamine is vital in the neuronal synthesis of neurotransmitters glutamate and GABA.
Astrocytes are also crucial in neurotransmitter recycling, critical for maintaining synaptic transmission. Thus, infection of the astrocytes could affect neuronal function, affecting synaptic function and plasticity.
In addition, infection of astrocytes also results in more significant neuronal death. This may partly explain the changes in the cortical thickness. Changes in the gray matter have been observed before in COVID-19 patients that were hospitalized. However, in this study, changes were observed in patients that had mild disease, suggesting even mild infection can impair brain functions.
The changes were related to anxiety and cognition, indicating the virus affected the cortical region of the brain. The authors speculate that because one of how the virus affects nerves is via the olfactory nerves, it is possible that the effect of the virus on the cortical regions could be because it is closely associated with the olfactory nerves.
Thus, the authors write, “Our study comes as a cautionary note that interventions directed to treat COVID-19 should also envision ways to prevent SARS-CoV-2 invasion of the CNS and/or replication in astrocytes.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Crunfli, F. et al. (2020) SARS-CoV-2 infects brain astrocytes of COVID-19 patients and impairs neuronal viability. medRxiv. https://doi.org/10.1101/2020.10.09.20207464, https://www.medrxiv.org/content/10.1101/2020.10.09.20207464v1
- Peer reviewed and published scientific report.
Crunfli, Fernanda, Victor C. Carregari, Flavio P. Veras, Lucas S. Silva, Mateus Henrique Nogueira, André Saraiva Leão Marcelo Antunes, Pedro Henrique Vendramini, et al. 2022. “Morphological, Cellular, and Molecular Basis of Brain Infection in COVID-19 Patients.” Proceedings of the National Academy of Sciences of the United States of America 119 (35): e2200960119. https://doi.org/10.1073/pnas.2200960119. https://www.pnas.org/doi/full/10.1073/pnas.2200960119.