Three lethal human respiratory syndromes associated with coronavirus (CoV) infections have emerged in the past two decades. They are severe acute respiratory syndrome (SARS) in 2002, Middle East respiratory syndrome (MERS) in 2012, and coronavirus disease 2019 (COVID-19) in 2019.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of COVID-19, is closely related to SARS-CoV-1 and MERS coronaviruses, which were more deadly but less transmissible than SARS-CoV-2.
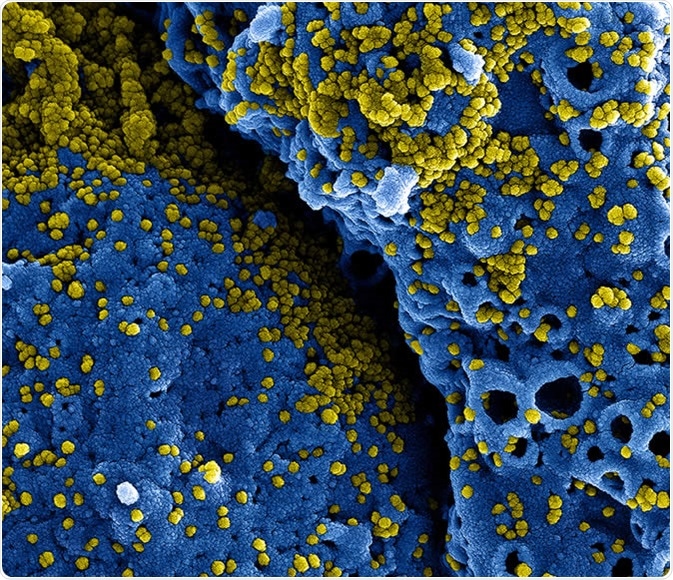
MERS Coronavirus Particles Colorized scanning electron micrograph of MERS virus particles (yellow) both budding and attached to the surface of infected VERO E6 cells (blue). Image captured and color-enhanced at the NIAID Integrated Research Facility in Fort Detrick, Maryland. Credit: NIAID
The ongoing COVID-19 pandemic has affected over 39.8 million lives globally and caused more than 1.11 million deaths so far. The pandemic has triggered crippling socio-economic repercussions in many nations across the globe. COVID-19 symptoms vary widely based on several factors and can lead to prolonged and severe illness in some patients. Some studies suggest that symptoms may persist even after recovery and negative real-time polymerase chain reaction (RT-PCR) test results.
This unprecedented challenge posed by COVID-19 has prompted extensive efforts to develop a vaccine and repurposed antiviral therapeutics that could offer potential treatments with known safety profiles and shorter timelines for development. The repurposing of Remdesivir, the antiviral nucleoside analog, and the anti-inflammatory steroid dexamethasone have given hope that existing compounds can be crucial in the fight against the COVID-19 pandemic. Despite this, there is still no approved treatment for COVID-19, and the efforts to find a vaccine or drug could be complicated by the evolution of SARS-CoV-2 and potential drug resistance it may achieve during evolution.
.jpg)
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (pink) heavily infected with SARS-COV-2 virus particles (green), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Comparing viral and human protein interactions of the three coronaviruses
A large team of researchers from various universities and institutes across the United States and Europe performed a comparative analysis of the interaction between viral and human proteins and the localization of viral protein for all three viruses. Their study is published in Science Magazine, the American Association's prestigious academic journal for advancing science.
The researchers conducted functional genetic screening and identified host factors that functionally interrupt the proliferation of coronavirus. These factors included a mitochondrial chaperone protein Tom70 that interacts with both SARS-CoV-1 and SARS-CoV-2 Orf9b. This interaction was structurally characterized with the help of cryo Electron Microscopy.
Differential interaction scoring approach identified virus-specific and shared interactions.
The researchers developed and compared three different coronavirus-host protein-protein interaction maps to identify and study pan-coronavirus molecular mechanisms. They used the quantitative differential interaction scoring (DIS) approach to identify virus-specific and shared interactions among different coronaviruses. They also systematically performed subcellular localization analysis with tagged viral proteins and antibodies that target specific proteins of
SARS-CoV-2.
The researchers identified key molecular mechanisms and potential therapeutic treatments by combining genetically validated host factors with genetic data from COVID-19 patients and medical records. Their results showed that protein localization could differ when individually expressed viral proteins are compared with that same protein's localization during infection. This may be due to many factors, including tagging-driven miss-location, localization changes due to interaction partners, or cellular compartments specific to the infection.
“Replication in other patient cohorts and further work will be needed to see if there is therapeutic value in these connections, but at the very least we have demonstrated a strategy wherein protein network analyses can be used to make testable predictions from real-world, clinical information.”
These differences are crucial caveats of host-viral interaction studies performed using tagged expressed proteins. However, this work and previous studies show how these observations are critical for identifying host targeted processes and appropriate drug targets. The authors feel that their results are significant enough to merit further molecular and clinical studies.
An integrative approach to analyze and understand coronavirus infection
Overall, the researchers described a collaborative and integrative approach to study and interpret coronavirus infection and identify targeted mechanisms that can be of high relevance for other coronavirus family viruses. They used various techniques from proteomics, virology, cell biology, genetics, biochemistry, structural biology, and clinical and genomic information to offer a holistic view of the interactions of SARS-CoV-2 and other coronaviruses with the infected host cells. The researchers strongly recommend using such an integrative approach to study other infectious agents and other disease areas.
“Although a careful analysis of the relative benefits and risks of typical antipsychotics should be undertaken before considering prospective studies or interventions, these data and analysis demonstrate how molecular information can be translated into real-world implications for the treatment of COVID-19, an approach that can ultimately be applied to other diseases in the future.”