Melatonin is a neurohormone produced in the brain (mainly at night) that prepares the body for sleep and is, therefore, sometimes referred to as the "sleep hormone."
In a retrospective analysis of patients who sought care at New York-Presbyterian/Columbia University Irving Medical Center, Nicholas Tatonetti and colleagues found exposure to melatonin following endotracheal intubation was significantly associated with a positive survival outcome in both COVID-19 and non-COVID-19 patients.
Furthermore, melatonin exposure following intubation was also associated with a positive survival outcome among patients with COVID-19 who required mechanical ventilation. However, no such benefit was observed among non-COVID-19 patients who required mechanical ventilation.
The authors say this suggests that melatonin may target severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-induced inflammation in the most severe cases of COVID-19.
The team says further studies are needed to investigate the possible mechanisms underlying these observations.
A pre-print version of the paper is available on the server medRxiv*, while the article undergoes peer review.
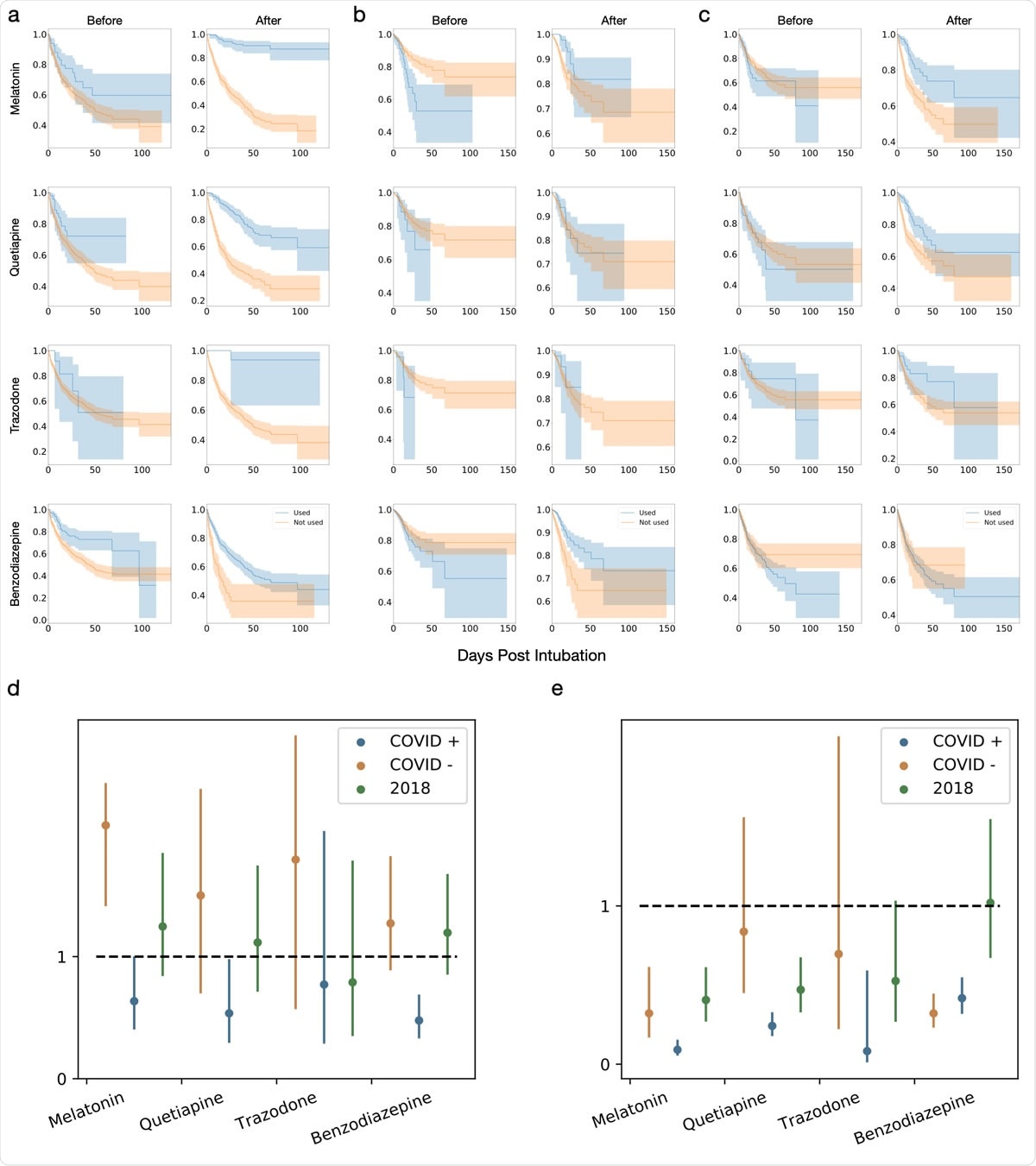
a-c Kaplan-Meier curves for melatonin, quetiapine, trazodone and benzodiazepines treatment before and after intubation for (a) COVID-19 intubation periods, (b) non-COVID-19 intubation periods and (c) intubation periods from 2018. d,e. Comparison of hazard ratios for melatonin, quetiapine, trazodone and benzodiazepines exposure (d) before and (e) after intubation.
Respiratory distress is the most serious COVID-19 symptom
Following infection with SARS-CoV-2, most people commonly develop symptoms including fever, cough, fatigue, shortness of breath, and loss of taste or smell. However, less common and more severe symptoms that are influenced by the presence of comorbidities can also develop.
The most severe symptom is respiratory distress, which, in the most severe cases, may require endotracheal intubation, mechanical ventilation, and potentially even lung transplant.
Among the candidate therapies that researchers have been investigating for the treatment of COVID-19, hormone drugs such as dexamethasone have shown promising results. A study of dexamethasone carried out by the RECOVERY Collaborative Group in the UK found that compared with usual care, treatment with dexamethasone lowered the mortality rate among patients who required invasive mechanical ventilation and patients who received oxygen without mechanical ventilation.
What did the current study involve?
In a retrospective study of 189,987 patients who sought care at NYP/CUIMC between February 1st, 2020, and August 1st, 2020, Tatonetti and colleagues used survival analysis to determine whether exposure to the "sleep hormone" melatonin following intubation was associated with mortality among intubated and mechanically ventilated patients.
The team identified 948 periods of intubation periods across 791 patients who had COVID-19 or were infected with SARS-CoV2 and 3,497 intubation periods across 2,981 patients who did not have COVID-19 or SARS-CoV-2.
A multivariate analysis that accounted for demographic factors and clinical diagnoses revealed that melatonin exposure following intubation was significantly associated with a positive survival outcome among both COVID-19 patients and non-COVID-19 patients.
Furthermore, melatonin exposure following intubation was also significantly associated with a positive survival outcome among mechanically ventilated COVID-19 patients, but not among mechanically ventilated patients who did not have COVID-19.
Clues about the underlying mechanism of action involved
"While our analysis identified significant associations between melatonin exposure after intubation and survival, we have not identified the directionality nor the underlying mechanism," says the team.
However, the association between exposure to melatonin following intubation and patient survival in a multivariate model of COVID-19 and non-COVID-19 patients suggests that melatonin exposure does not specifically attenuate inflammation that arises from SARS-CoV-2 infection, say the researchers.
On the other hand, the fact that exposure to melatonin following intubation that also required mechanical ventilation was only associated with a positive outcome in COVID-19 patients suggests that melatonin's mechanism of action in the most severe cases of COVID-19 may be targeted to SARS-CoV-2 induced inflammation, adds the team.
"While melatonin is a popular over-the-counter sleep aid, our results lend support to the need for further follow-up into the mechanism of action of how melatonin may attenuate inflammation and specifically more studies into the observed association in severely affected COVID-19 patients," conclude Tatonetti and colleagues.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.