Image Credit: Corona Borealis Studio / Shutterstock
Background
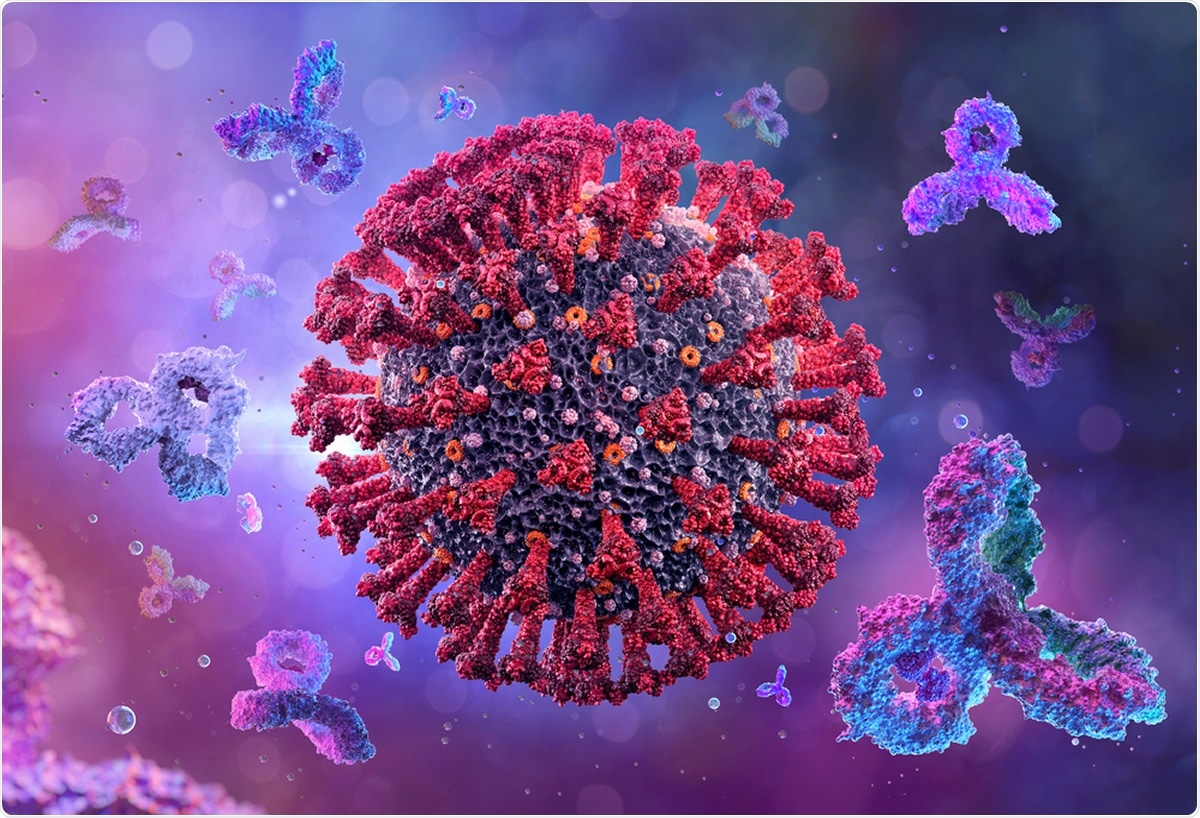
There have been studies that have shown that antibody responses to severe COVID-19 are well defined. Even mild and asymptomatic cases have shown good antibody responses. Researchers write that since these mild and asymptomatic cases form a majority of the cases, this finding is a vital one.
However, there is a need to determine the robustness of this antibody response and its longevity and functionality in the body, the team explains. Serological surveys (or sero surveys) are being conducted around the world to determine the levels as well as the duration of the antibody titers (or concentration of effective antibodies) in the body that could protect against re-infection with SARS-CoV-2.
Antibodies
Researchers explained that antibodies to SARS-CoV-2 basically develop against one or more of its protein components. These encoding proteins of the virus are both structural and non-structural antigens.
At present, there are two structural proteins that act as antigens and stimulate antibodies which can be detected on sero surveys. These are - nucleoprotein (NP) and spike protein.
The NP is found in adequate amounts within the virus or in infected cells. It is usually protected by the virus membranes and thus antibodies to NP are not commonly detected. Antibodies to NP cannot neutralize the virus.
The spike protein is, on the other hand, a large protein on the viral surface. It is a trimeric glycoprotein that has a region called the “receptor binding domain (RBD).” The RBD binds to the receptor angiotensin-converting enzyme 2 (ACE2) on the cell of the humans that allows the virus to penetrate the cell and cause infection. Antibodies develop to the spike protein and thus can be measured through sero surveys.
Tests for serological surveys
At present the most common and most used test is the Mount Sinai ELISA (enzyme-linked immunosorbent assay) that has a high sensitivity – that is, chances of detecting true positives 92.5 percent - and specificity - chances of detecting true negatives 100 percent. This test has a positive predictive value (PPV) of 100 percent, with a negative predictive value (NPV) of 99.6 percent, making it robust and reliable.
Study design
Screening for antibody response began at the Mount Sinai Health System in March 2020. This was initially done to screen for volunteers would be able to donate plasma for convalescent plasma therapy in patients with, or recovering from, severe COVID-19. These potential donors had been detected earlier with COVID-19 on RT PCR.
A large number of people were screened. Of these, only 5 percent needed hospitalization for COVID-19 earlier. The researchers wrote that from March to October 2020, they had screened 72,401 individuals for antibodies, and of these, 30,082 individuals had detectable levels of antibodies.
The researchers’ definition of detectable antibodies were detectible to the spike protein at a titer of 1:80 or higher. Titers of 1:80, 1:160, 1:320, 1:960, or ≥1:2880 were defined, and those with 1:80 and 1:160 were categorized as low titers. Those with 1:320 were defined as moderate, and those with tites of 1:960 and ≥1:2880 were classified as high titers. Plasma donors were eligible with tires of 1:320 or higher.
Results
Antibody response
From the antibodies screening, the following results were seen among the 30,082 positive samples:
- 690 (2.29 percent) had a titer of 1:80
- 1,453 (4.83 percent) had a titer of 1:160
- 6,765 (22.49 percent) had a titer of 1:320
- 9,564 (31.79 percent) had a titer of 1:960
- 11,610 (38.60 percent) had a titer of 1:2880
The researchers found that a “vast majority” of positive individuals had “moderate-to-high titers of anti-spike antibodies.”
The team then analyzed 568 individuals who had been confirmed as COVID-19 positive. Among them, over 99 percent developed anti-spike antibodies. A further 95 percent of 2,347 patients who had reported that they had earlier tested positive for COVID-19 showed positive antibody titers.
Longevity of the antibodies
To assess this the team recalled 121 volunteers who had been eligible earlier as plasma donors. The population was tested approximately 30 days after the onset of symptoms and also again at two additional points in time.
The average interval between the initial measurement and the second was 52 days, but ranged between 33 and 57 days. The second measurement was an average of 82 days after onset of symptoms but ranged between 52 and 104 days after symptoms onset. A third measurement was made at an average of 148 days after symptom onset (but ranged between 113 and 186 days).
Overall results were
- The geometric mean titer (GMT) fell from 764 to 690 between first and second measurement
- The GMT fell to 404 at third measurement
- Those who had high tires of 1:2880 and 1:960 saw a slower decline in titer with time
- Those with initial titer of 1:320, 1:160, or 1:80 saw a fall on day 30, which persisted till day 148.
- The team found that the half-life of the antibody IgG is approximately 21 days. This sustenance of the antibodies shows that it is possibly due to “long-lived plasma cells in the bone marrow”
Conclusions and implications
Overall, the researchers found that the protective duration from SARS-CoV-2 is not clear from previous studies. Their own study shows that individuals who have recovered from mild COVID-19 have developed robust antibody responses to the spike protein that seems to last. Stable antibody response is seen for at least three months, and only modest declines are seen at five months. A future follow up of the participants would show the longevity and functionality of these antibodies, the team has observed.
They found that “A correlate of protection, combined with a better understanding of antibody kinetics to the spike protein, would inform policy regarding the COVID-19 pandemic and would be beneficial to vaccine development efforts.”