A team of researchers has conducted a study suggesting that the majority of the global population is likely to have pre-existing T-cell immunity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent responsible for the coronavirus disease 2019 (COVID-19) pandemic.
The team – from the United States and India – says many people who have not yet been exposed to the virus probably already have SARS-CoV-2-reactive T cells as a result of previous exposure to viruses such as influenza and cytomegalovirus (CMV).
The researchers say the study demonstrates that strong immunity among unexposed individuals can arise through cross-reactive T cell receptors (TCRs) against common CMV and influenza antigens that mount an early CD8 T-cell response to clear SARS-CoV-2.
“This finding is in contrast to multiple published studies in which pre-existing T-cell immunity is suggested to arise from shared epitopes between SARS-CoV-2 and other common cold-causing coronaviruses,” say Amitabha Chaudhuri from MedGenome in Foster City, United States and colleagues from MedGenome in Bangalore, India.
A pre-print version of the paper is available on the server bioRxiv*, while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
SARS-CoV-2 disease phenotypes vary widely
Since the first cases of COVID-19 were identified in Wuhan, China, late last year (2019), a range of disease phenotypes have been observed, ranging from asymptomatic or mild, to severe clinical outcomes and death.
Understanding the underlying immunological mechanisms that give rise to such different disease phenotypes would aid the development of next-generation therapies and the management of critically ill COVID-19 patients.
Many studies have previously shown that CD8 T cell immunity is required for the clearance of respiratory viruses. Delays in CD8 T-cell activation and the production of interferon-g (IFN-g) results in high viral loads that trigger overactivation of the innate and adaptive immune responses.
This can lead to dysregulation in immune homeostasis that gives rise to a severe disease phenotype.
“Therefore, an early wave of strong CD8 T-cell response may delay viral titer build-up, allowing rapid clearance of the virus by the immune system without perturbing immune homeostasis,” write the researchers.
Studies have shown that healthy individuals not yet exposed to SARS-CoV-2 exhibit pre-existing CD4 and CD8 T-cell immunity to the virus. Some studies have also suggested that a pool of SARS-CoV-2-reactive T-cells arises in unexposed individuals who have previously been infected with human coronaviruses that cause the common cold.
However, whether this pre-existing immunity protects against SARS-CoV-2 infection or contributes to a faster recovery following infection, remains unclear.
It also remains unclear whether such pre-existing immunity, involving either CD4 or CD8 T-cells, or both, is required for maximal protection, adds the team.
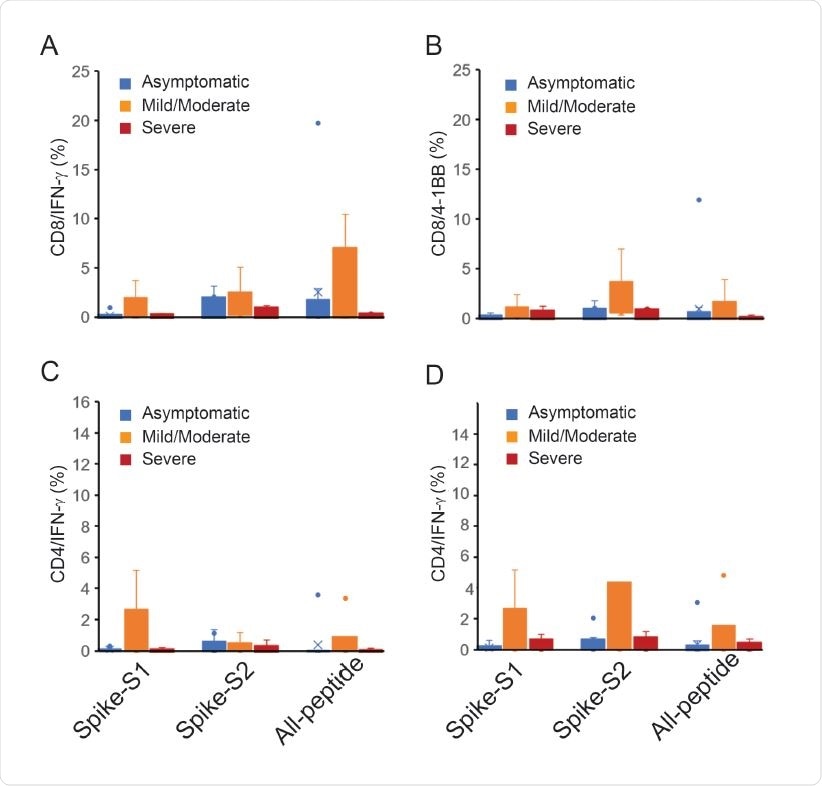
T-cell reactivity to Spike-S1, S2 pools and 11-peptide-mix in asymptomatic, mild-moderate and severe disease after in vitro stimulation for 48 h. A. IFN-γ and 4-1BB expression in activated CD8 T-cells. B. IFN-γ and 4-1BB expression in activated CD4 T-cells.
What did the current study involve?
Chaudhuri and colleagues developed a novel TCR-binding algorithm called OncoPeptVAC that predicts CD8 T-cell activating epitopes across the SARS-CoV-2 proteome.
The algorithm identified many CD8 T-cell epitopes in a small pool of 11 peptides that are used in assays of T-cell activation.
This 11-peptide pool was tested for T-cell activation in healthy individuals from the United States and India who had not been exposed to SARS-CoV-2.
The pool of predicted epitopes triggered robust T-cell activation, suggesting that the unexposed individuals already had CD4 and CD8 T-cell immunity to the virus.
However, homology analysis indicated a lack of significant amino acid identity between the 11 peptides and the antigens of other human coronaviruses.
The researchers say this suggests “engagement of one or more peptides in the pool to cross-reactive TCRs from other viruses, not particularly from a coronavirus.”
Further TCR analysis identified expanded clonotypes that recognize epitopes from common viruses such as influenza-A and CMV.
What are the implications of the findings?
“Our study uncovered strong pre-existing CD8 T-cell immunity [against SARS-CoV-2] using a small set of 11 epitopes that engaged cross-reactive TCRs recognizing epitopes from other viruses, not necessarily common cold viruses belonging to the coronavirus family as hypothesized by other studies,” write Chaudhuri and colleagues.
The researchers say the findings raise the expectation that a significant majority of the global population is likely to have SARS-CoV-2 reactive T-cells as a result of previous exposure to influenza and CMV, as well as exposure to common cold-causing coronaviruses.
“Identifying additional immunodominant epitopes in SARS-CoV-2 and their cognate TCRs can become a powerful immune monitoring tool for assessing protective immunity against SARS-CoV-2 in the population,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Chaudhuri A, et al. Immunodominant T-cell epitopes from the SARS-CoV-2 spike antigen reveal robust pre-existing T-cell immunity in unexposed individuals. bioRxiv, 2020. doi: https://doi.org/10.1101/2020.11.03.367375, https://www.biorxiv.org/content/10.1101/2020.11.03.367375v1
- Peer reviewed and published scientific report.
Mahajan, Swapnil, Vasumathi Kode, Keshav Bhojak, Coral Karunakaran, Kayla Lee, Malini Manoharan, Athulya Ramesh, et al. 2021. “Immunodominant T-Cell Epitopes from the SARS-CoV-2 Spike Antigen Reveal Robust Pre-Existing T-Cell Immunity in Unexposed Individuals.” Scientific Reports 11 (1). https://doi.org/10.1038/s41598-021-92521-4. https://www.nature.com/articles/s41598-021-92521-4.