With the COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infecting over 50 million people worldwide with hundreds of thousands experiencing severe respiratory illness, researchers have been trying to find the factors associated with severe disease. From the start of the pandemic in March this year, several studies have indicated heart disease, high blood pressure, diabetes, obesity, etc. could be linked to severe disease.
Now German researchers have published a study on the association between severe respiratory infection caused by SARS CoV-2 and factors such as age, body mass index (BMI) and ABO blood group. Their study titled, "Severity of Respiratory Infections due to SARS-CoV-2 in Working Population: Age and Body Mass Index Outweigh ABO Blood Group," was released prior to peer review on the preprint site medRxiv*.
Background
There is a rise in cases of COVID-19, and there is a lack of consensus regarding the high-risk factors for severe disease course.
The authors of the study write that with the rising number of cases, Germany reintroduced lockdown measures to reduce the risk of spread of the infection. The main question is to identify those at greater risk, such as the elderly, and protect them from the infection. While the elderly are identified to be at risk, the risk among the working population is not yet defined.
The stem cell registry
As part of the DKMS gemeinnützige GmbH (DKMS), a major stem cell donor registry, tens of millions of volunteers report their general health conditions and medical details. The volunteers were adults aged below 61 years, wrote the researchers.
During the pandemic, the DKMS launched a large population-based study to identify risk factors that could lead to severe COVID-19.
Blood group
Some initial studies have shown that blood group A may raise the risk of contracting the virus and also carries a risk of more severe disease. The cause for this is not clear. Some studies showed that the A epitopes in blood could facilitate the virus's entry into the host cells.
ABO epitopes are known to alter and change several proteins, lipids and sphingolipids. Those who have at least 1 A1 allele, write the researchers, could have higher glycosyltransferase activity, which could raise the risk of getting the infection.
In this study, the team of researchers looked at the risk of infection among those with A1 phenotype compared to those with A2 phenotype.
Age and body mass index (BMI)
Studies have shown that increasing age and obesity could be risk factors for getting severe COVID-19.
Study design
The participants in this study were those part of the DKMS aged between 18 and 61 years. From the participants, nasopharyngeal swabs to detect COVID-19 were gathered, and all health-related data were analyzed. Risk factors, symptoms of the infection, treatment course, and final outcome were collated. A health questionnaire was used to gather further information. Logistic regression models were used to assess the risk of contracting SARS-CoV-2 as well as the risk of severe respiratory infection and risk of hospitalization.
A total of 4,440,895 donors were contacted between August 17th, 2020, and August 26th, 2020. Participants who had been tested but never tested positive for SARS-CoV-2 were assigned as negative cases. Participants testing positive were classified as:
- Those with severe respiratory tract infections (RTI). This was defined as a combination of at least "fever and cough", "dyspnea (difficulty in breathing) and cough", "dyspnea and fever", or "dyspnea and myalgia (body ache)". This group included those who needed hospitalizations due to respiratory complications. Hospitalization was defined as "in-patient care with supplemental oxygen or mechanical ventilation or hospitalization for dyspnea or cough."
- Those with mild/moderate disease with self-reported symptoms not meeting the above definition. Their symptoms included "fever, myalgia, sore throat, loss of taste/smell, cough, or dyspnea."
- Asymptomatic participants
ABO and Rh blood grouping was done, and genetic analysis was performed using buccal swabs. Participants were grouped as per alleles as:
- Blood group A1 – A1+0, A1+A1, A1+A2, A1+A3, A1+Aw, or A1+Ax
- Blood group A2 - A2+0, A2+A2, A2+Ax, orA2+Ael
Results:
The findings of the study were as follows:
- A total of 924,660 individuals finally participated in the study
- 7,948 of these had tested positive for SARS-CoV-2
- Severity of course of the infection:
- 947 participants (11.9 percent) were asymptomatic for the infection
- 5,014 (63.1 percent) had a mild/moderate respiratory course of the disease
- 1,987 (25 percent) had severe respiratory tract infections
- 286 participants (3.6 percent) were hospitalized for respiratory tract infections
- When compared with normal body weight, those with higher BMI had a higher risk of hospitalization. Participants with BMI ≥ 40 had a 3.2-fold greater risk (95%-CI: 1.6 to 6.7; of respiratory hospitalizations compared to individuals with normal weight. The risk was as follows:
- BMI 35 to 40 Kg/mg2 - The risk was 2.1-fold higher (95%-CI, 1.2-3.69, p=0.01) compared to normal weight person aged 20 years.
- BMI 35 to 40 Kg/mg2 - The risk was 11.2-fold higher (95%-CI, 10.1-14.6, p<0.001) compared to a normal-weight person aged 55 years.
- Participants aged 55 to 61 years had a 5.3-fold greater risk (95%-CI: 2.9-9.7 for respiratory hospitalizations compared to participants aged 18 to 24 years.
- The risks for respiratory hospitalizations for participants with a history of diabetes or arterial hypertension was not raised significantly (odds ratios of 1.62 and 1.26, respectively)
- Blood group A was associated with a 1.15-fold higher risk for contracting COVID-19 (95%-CI 1.08-1.22, p<0.001) compared to blood group O.
- Participants with A1 and A2 phenotypes had similar rates of positive tests (5.3% and 5.4%, adjusted OR 1.03, 95%-CI 0.93-1.15; p=0.58).
- Blood group A did not raise the risk of severe COVID-19.
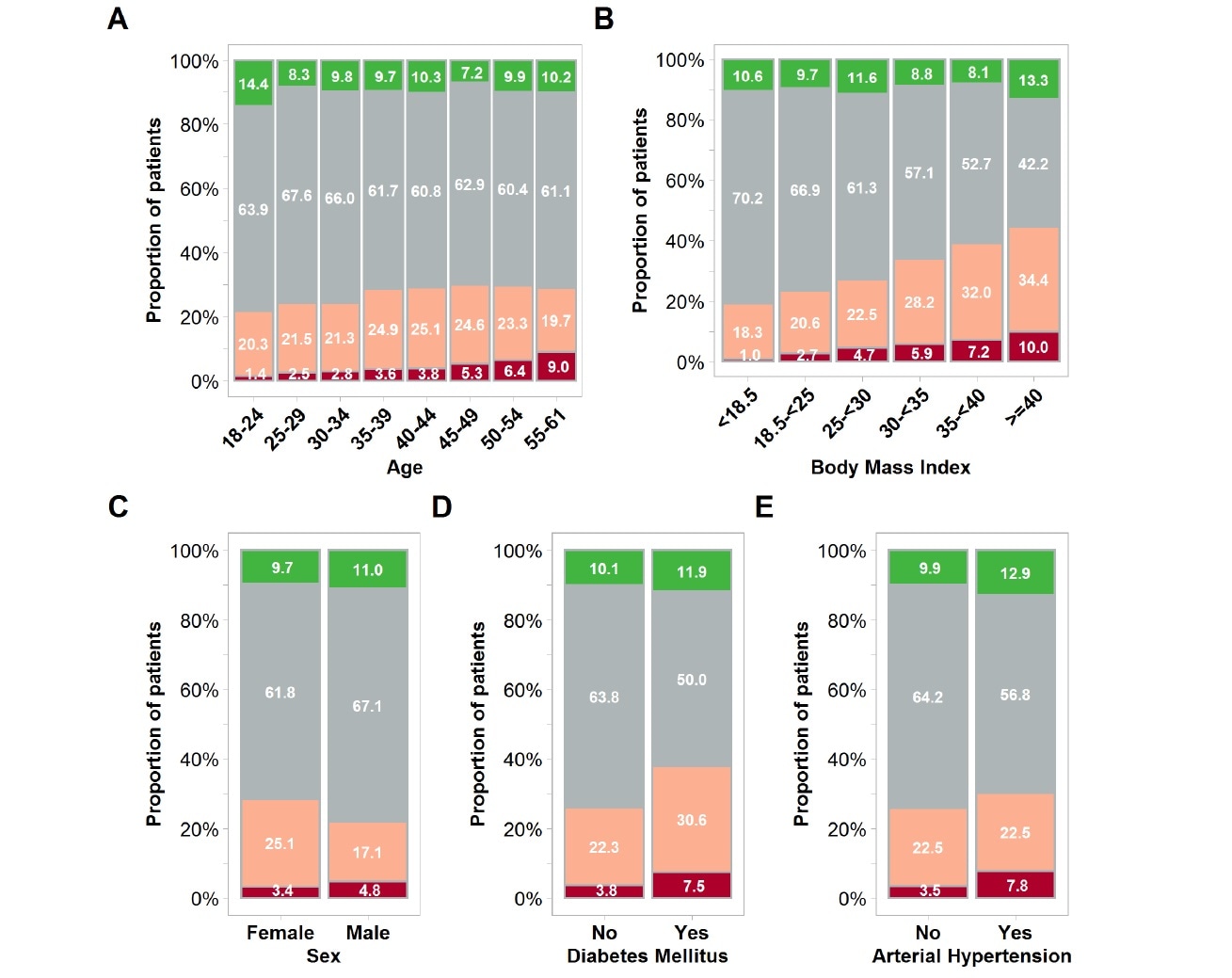
The severity of self-reported COVID-19 courses is shown for all individuals who reported a positive test for SARS-CoV-2 from an oro- or nasopharyngeal swab between January and July. Results are shown by age group (Panel A), body mass index (Panel B), sex (Panel C), diabetes medication (Panel D), and arterial hypertension medication (Panel E). Red color indicates respiratory hospitalizations, defined by in-patient care with supplemental oxygen or mechanical ventilation or hospitalization for dyspnea or cough. Rose color indicates severe respiratory tract infections defined by the combination of at least fever and cough, dyspnea and cough, dyspnea and fever, or dyspnea and myalgia, but no need for hospitalization. Gray color represents mild/moderate courses. These participants did not meet the criteria for severe respiratory tract infections but reported symptoms such as fever, myalgia, sore throat, loss of taste/smell, cough, or dyspnea.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Implications of the study findings
Authors write that this large study shows that hospitalizations risk due to SARS-CoV-2 infections were moderate among the healthy working population. Age and BMI remained significant risk factors. The authors wrote blood group A had no impact on the risk of hospitalization. They called for risk-stratified preventive measures to reduce risk and recommended individual counseling for risk mitigation.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.