The COVID-19 pandemic has become one of the deadliest pandemics in modern history. Since its emergence in late December 2019, the highly infectious severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen for COVID-19, has infected more than 55.5 million people and claimed more than 1.33 million lives globally. Although the majority of COVID-19 patients remain asymptomatic or mildly symptomatic, older adults and people with comorbidities (hypertension, cardiopulmonary disorders, diabetes, and renal disorders) are highly susceptible to develop life-threatening SARS-CoV-2 infection.
Of various COVID-19 related complications, cardiac abnormalities have been noticed in about 25% of patients. Such complications are associated with a significantly higher mortality rate. In most hospitalized COVID-19 patients, an increased troponin level is considered the main determining factor for cardiovascular abnormalities. Cardiovascular injuries can occur in COVID-19 patients because of many factors, such as elevated levels of proinflammatory mediators, coagulation/thrombosis-mediated microvascular damage, and a drop in blood oxygen level combination with disease-induced higher metabolic demand, or direct viral entry into myocardial cells. To gain more insight into cardiac complications of COVID-19 patients, a systematic evaluation of electrocardiography (ECG) findings can be an effective approach.
Given the proven prognostic value of ECG and its easy availability, the current study scientists tried to find out whether ECG findings of COVID-19 patients stratified by troponin levels can better predict the cardiovascular scenario and prognosis of hospitalized COVID-19 patients.
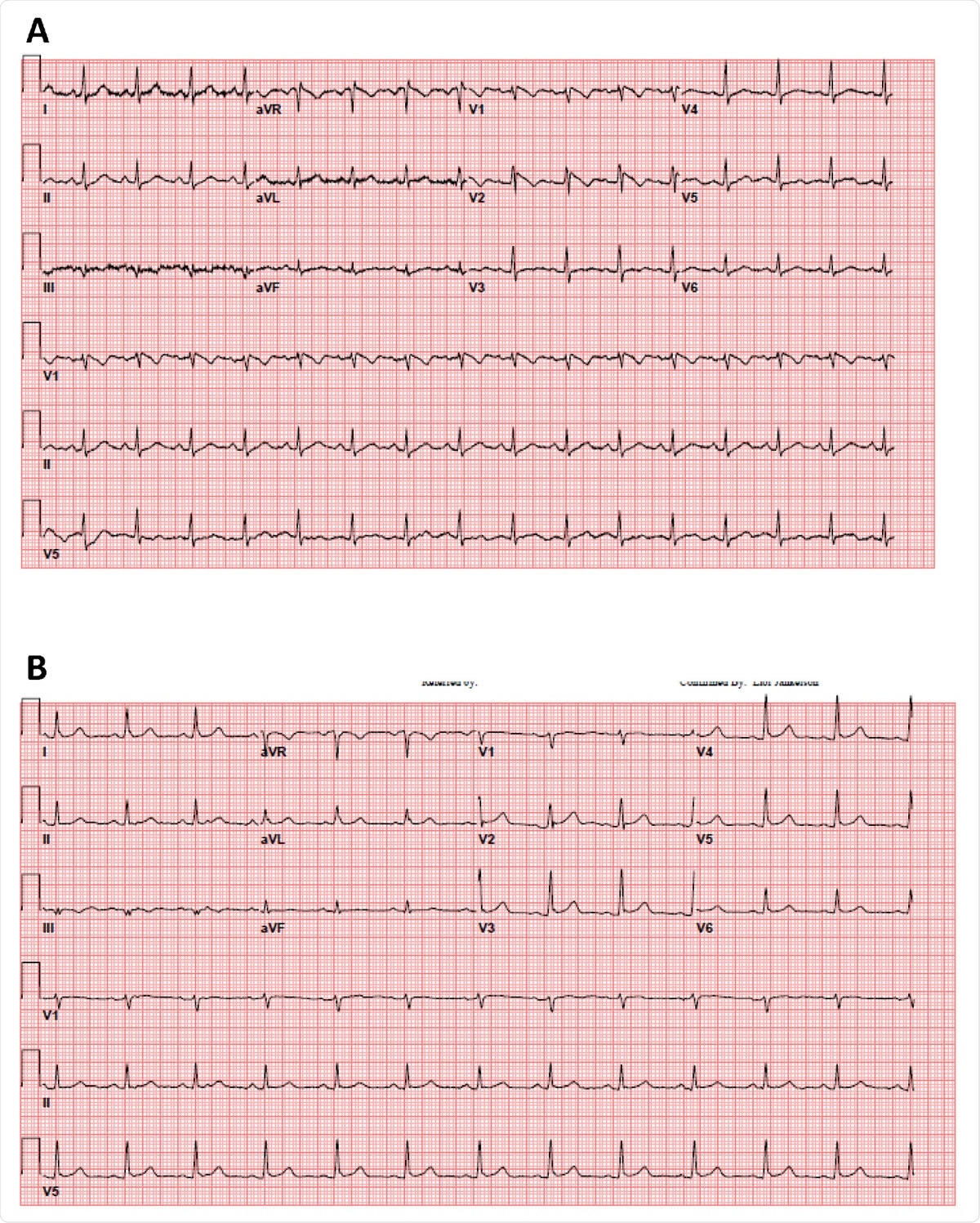
35 year old female patient without significant medical history presented with a fever of 103.1 F. A. The patient’s initial 12-lead electrocardiogram in the emergency department. B. The patient’s repeat 12-lead electrocardiogram with resolution of fever.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Current study design
The study was conducted on 204 adult COVID-19 patients admitted at New York University Langone Medical Center, USA. The patient’s baseline characteristics, laboratory findings, and ECG findings were obtained from the medical reports. The blood level of troponin I was assessed and grouped into normal (≤0.05 ng/ml), mildly increased (≥0.05 ng/ml), and severely increased (>1 ng/ml). Five eminent cardiologists analyzed various ECG findings, including heart rate, cardiac rhythms, right/left bundle branch block, atrioventricular block, and repolarization abnormalities (ST elevation/depression, or T wave inversion).
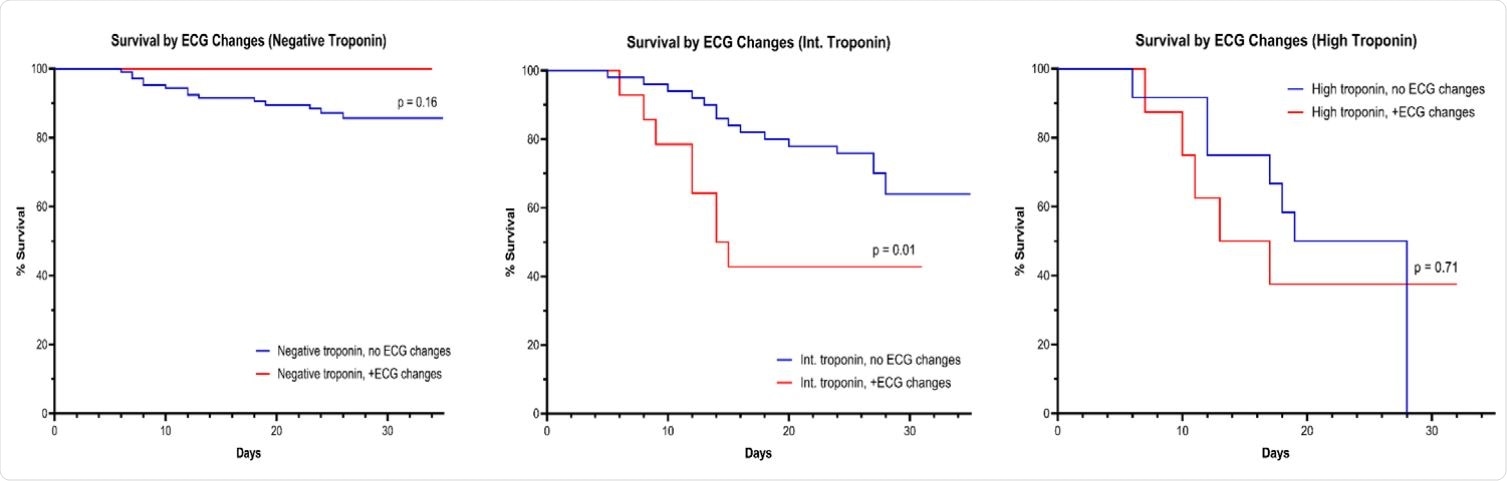
KM survival according to ECG changes stratified by Troponin elevation group
Important observations
Regarding comorbidities of studied patients, hypertension was the most common one (56%), followed by diabetes (30%), coronary artery disease (12%), chronic obstructive pulmonary disease (6%), and heart failure (3%).
Regarding baseline ECG findings, the most common abnormalities were ST elevation, ST depression, and T wave inversion. Normal sinus rhythm was observed in most of the patients, with only 5% showing atrial fibrillation.
After stratifying ECG findings with troponin data, the scientists observed that repolarization abnormalities were significantly correlated with higher troponin levels. Moreover, they observed that patients with both repolarization abnormalities and higher troponin levels are at higher risk of COVID-19 related mortality.
Further statistical analysis revealed that age and increased troponin level were the main predictors of death due to COVID-19 related problems, such as respiratory complications or multiorgan failure. A direct correlation was observed between the mortality rate and increased troponin level. About 38% and 60% of patients who died of COVID-19 related complications showed mildly increased and severely increased troponin levels, respectively.
Interestingly, in patients with mildly increased troponin levels, ECG abnormalities were associated with significantly higher COVID-19 related deaths.
Study significance
Although severely increased troponin level is frequently used to define cardiac injury in hospitalized COVID-19 patients, the current study findings revealed that the majority of COVID-19 patients displayed low (59%) or mildly higher (31%) troponin levels. In contrast, only 10% of studied patients displayed severely higher troponin levels. However, patients with severely increased troponin levels are more susceptible to COVID-19 related death.
The most important finding of the study is that in patients with mildly increased troponin levels, the risk of death can be predicted by assessing ECG abnormalities.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Electrocardiographic Abnormalities and Troponin Elevation in COVID-19 Ehud Chorin, Matthew Dai, Edward Kogan, Lalit Wadhwani, Eric Shulman, Charles Nadeau-Routhier, Robert Knotts, Roi Bar-Cohen, Chirag Barbhaiya, Anthony Aizer, Douglas Holmes, Scott Bernstein, Michael Spinelli, David Park, Larry Chinitz, Lior Jankelosn medRxiv 2020.11.12.20230565; doi: https://doi.org/10.1101/2020.11.12.20230565 https://www.medrxiv.org/content/10.1101/2020.11.12.20230565v1
- Peer reviewed and published scientific report.
Chorin, Ehud, Matthew Dai, Edward Kogan, Lalit Wadhwani, Eric Shulman, Charles Nadeau-Routhier, Robert Knotts, et al. 2021. “Electrocardiographic Risk Stratification in COVID-19 Patients.” Frontiers in Cardiovascular Medicine 8 (February). https://doi.org/10.3389/fcvm.2021.636073. https://www.frontiersin.org/articles/10.3389/fcvm.2021.636073/full.