Researchers in Singapore have conducted a study showing that asymptomatic individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19) – mount an efficient, balanced and coordinated cellular immune response that protects the host without appearing to trigger any pathological processes.
Compared with symptomatic disease, asymptomatic infection activated virus-specific T cells that produced higher levels of the cytokines interferon-γ (IFN-γ) and interleukin-2 (IL-2) and triggered more proportional secretion of inflammatory and regulatory cytokines.
Clarence Tam from the National University of Singapore and colleagues suggest that the ability of asymptomatic individuals to induce proportionate secretion of the cytokine IL-10 may help to reduce inflammatory events while they clear the virus.
A pre-print version of the paper is available on the bioRxiv* server while the article undergoes peer review.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Characterization of adaptive immunity is essential
Characterization of the adaptive immune response following SARS-CoV-2 infection is essential for understanding how it contributes to protective or pathological processes.
SARS-CoV-2-specific antibodies and T cells work together to reduce viral spread and eliminate the pathogen from infected cells. However, this protective immune response can also induce pathological processes such as inflammation and tissue damage following lysis of infected cells or their release of inflammatory mediators.
Studies have shown that in severe cases of COVID-19, high levels of inflammatory cytokines and the presence of activated monocytes in the lung co-exist with virus-specific T cells and antibodies.
“Thus, the question of whether virus-specific antibodies or T cells are preferentially mediating protection or damage remains open,” said Tam and colleagues.
Antibodies against a surface viral protein called spike, which SARS-CoV-2 uses to gain entry to host cells, have been shown to exhibit protective activity in vitro, but titers of these antibodies have also been associated with disease severity in patients with COVID-19.
Studies of SARS-CoV-2-specific T cells have also shown an association between the frequencies of these cells and disease severity in COVID-19 patients.
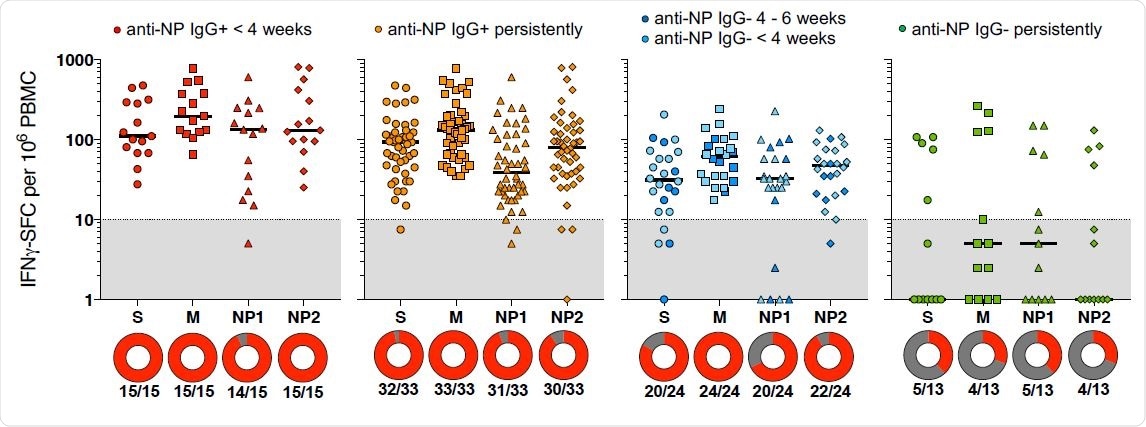
Frequency of T cells specific for different SARS-CoV-2 proteins in asymptomatic donors with distinct serological profiles. The frequency of IFN-γ-spot forming cells (SFC) reactive to the individual peptide pools is shown for the asymptomatic donors with distinct serological profiles (line = median). IFN-γ-SFC ≥10/106 PBMC were considered positive (grey area is below limit of detection). Circles below represent the percentage of a positive response (red) to the individual peptide pools.
Asymptomatic infection has been proposed to reduce antiviral adaptive immunity
Although infection is efficiently controlled in asymptomatic infection, it has been proposed that asymptomatic individuals mount a reduced antiviral adaptive immune response.
Studies have reported a lower magnitude of antibody and T cell responses in asymptomatic versus symptomatic individuals, which has been interpreted as indicative of a normal innate immune response, but a weak adaptive immune response.
However, the current knowledge regarding antiviral immunity in asymptomatic individuals is limited, say Tam and the team.
The researchers propose that asymptomatic individuals may hold the key to understanding how the immune response controls SARS-CoV-2 infection without causing pathology.
“SARS-CoV-2-specific T cells in individuals who clear SARS-CoV-2 infection without symptoms or disease could reveal non-pathological yet protective characteristics,” they write.
What did the researchers do?
The team compared the quantity and function of SARS-CoV-2-specific T cells among asymptomatic individuals and symptomatic COVID-19 patients.
The researchers quantified the secretion of a range of cytokines in whole blood following T cell activation with SARS-CoV-2 peptide pools.
“This experimental system not only measures the quantity of T cell cytokines (IL-2, IL-4, IFN-γ) directly secreted by SARS-CoV-2-specific T cells but can provide a direct evaluation of the T cells’ ability to activate inflammatory or regulatory pathways in other circulating immune cells,” says the team.
What did they find?
The overall magnitude of T cell responses against viral proteins during the early stages of recovery was similar between asymptomatic individuals and COVID-19 patients.
However, the T cells induced by asymptomatic infection secreted higher quantities of IFN-γ and IL-2 than those induced by symptomatic infection.
In asymptomatic individuals only, the team observed a proportional and coordinated secretion of the pro-inflammatory cytokines IL-6, TNF-α and IL-1β and the anti-inflammatory cytokine IL-10.
By contrast, the secretion of inflammatory cytokines in symptomatic individuals was disproportionate, say Tam and colleagues.
“Our results provide experimental evidence that asymptomatic individuals mount a virus-specific T cell response that is indistinguishable from symptomatic patients in magnitude, but that is functionally more fit,” they write.
Asymptomatic SARS-CoV-2 infection is therefore not characterized by a weak antiviral immunity; but rather a highly functional virus-specific cellular immune response, they add.
What are the study implications?
“The ability to induce a proportionate production of IL-10 might help to reduce inflammatory events during viral clearance,” suggests the team.
The researchers say that preclinical studies have already indicated that the simultaneous secretion of IFN-γ and IL-10 by T cells leads to effective viral control without inducing pathological processes.
They suggest that this could be the functional signature of protective virus-specific cellular immune responses in cases of asymptomatic SARS-CoV-2 infection.
“A detailed analysis at the single-cell level of the functional profile of SARS-CoV-2-specific T cells in symptomatically and asymptomatically infected individuals will be needed to formally demonstrate such hypothesis,” conclude Tam and colleagues.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Tam C, et al. Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection. bioRxiv, 2020. doi: https://doi.org/10.1101/2020.11.25.399139, https://www.biorxiv.org/content/10.1101/2020.11.25.399139v1
- Peer reviewed and published scientific report.
Le Bert, Nina, Hannah E. Clapham, Anthony T. Tan, Wan Ni Chia, Christine Y.L. Tham, Jane M. Lim, Kamini Kunasegaran, et al. 2021. “Highly Functional Virus-Specific Cellular Immune Response in Asymptomatic SARS-CoV-2 Infection.” The Journal of Experimental Medicine 218 (5). https://doi.org/10.1084/jem.20202617. https://rupress.org/jem/article/218/5/e20202617/211835/Highly-functional-virus-specific-cellular-immune.