My laboratory has been studying mammalian metabolism and hypoxia for over three decades, working with human triathletes as well as dolphins, narwhals, lions, bears, and more. In trying to answer the question ‘How do marine mammals hold their breath for so long?’, we have found that tolerance to hypoxia varies markedly among animals.
A deep-diving beaked whale can hold its breath for over three hours compared to a handful of minutes for humans! Unfortunately, humans are highly vulnerable to tissue damage when oxygen is lacking- which naturally made me wonder about the potential impacts of hypoxia that had been reported for COVID-19 patients.
What physiological adaptations enable marine mammals to tolerate low oxygen levels?
The list seems to be endless for marine mammals. This work has involved national and international scientists for decades, and we are still discovering new ways in which marine mammals are able to protect their tissues when oxygen is unavailable.
I put a partial table of the discoveries in our paper to give readers a sense of the incredible suite of hypoxia-related adaptations found in seals and whales. It begins with onboard storage of oxygen within oxygen-sensitive tissues, especially the brain and locomotor and cardiac muscles.
Marine mammals have up to 10 times the amount of oxygen-carrying myoglobin within their muscles compared to a dog or a human.
But there is so much more, for example, enhanced buffering capacities if tissues go anaerobic, spleens that can sequester oxygenated red blood cells, and dive responses to reduce tissue metabolic demands all help avoid hypoxia-related damage. It is remarkable, and a testament to what is necessary for protecting the most vital organs of the body from oxygen deprivation.
What is the Krogh principle and why is it relevant here?
August Krogh was a Danish scientist who won the Nobel Prize in Physiology and Medicine exactly 100 years ago. He worked on vascular and respiratory physiology, specifically the delivery of oxygen to tissues. He was also interested in how the physiological adaptations of model animals could help us understand basic biological principles for humans.
The Krogh Principle states that "for such a large number of problems there will be some animal of choice, or a few such animals, on which it can be most conveniently studied." It is the foundation of Comparative Physiology. I have used this powerful philosophy of scientific inquiry and applied it to the many animal species that I’ve studied over the years.
August Krogh is one of my scientific heroes, and his are the scientific shoulders that I stand on. To honor him on the anniversary of his Nobel Prize, the editors of Comparative Biochemistry and Physiology created a special edition of which our paper on hypoxia is a part. Rather than simply write a review about hypoxia, my co-author and I decided to use the Krogh Principle to determine what animals could tell us about surviving hypoxia associated with COVID-19.
Why is hypoxia so important in COVID-19?
Scientists are learning so much about the impacts of hypoxia as the pandemic progresses. What is becoming apparent is that hypoxia – a lack of oxygen – is central to many of the symptoms first responders have observed in patients. Brain fog, COVID toes, fatigue, as well as heart, brain, and lung damage all have an element of oxygen deprivation at their root.
The mechanisms may not be entirely worked out yet. Direct damage to the lung by the virus, the inflammation reaction of the body, and microvascular damage all seem to contribute to the problem of oxygen delivery in patients.
The bottom line, however, is that oxygen may be lacking in vital tissues. That is concerning given the relative lack of defenses to hypoxia in humans compared to other animals like deep-diving marine mammals.
How could this research benefit treatment and understanding of COVID-19 patients?
This answer relies on some really basic physiological principles for body tissues. Certain tissues, most notably the brain and heart of mammals are exceptionally oxygen-sensitive. This is problematic because these are also the most critical organs in our bodies.
Figure 4 in our paper addresses this, and in my opinion, is the most important illustration in our review. It says two very important things that people need to understand.
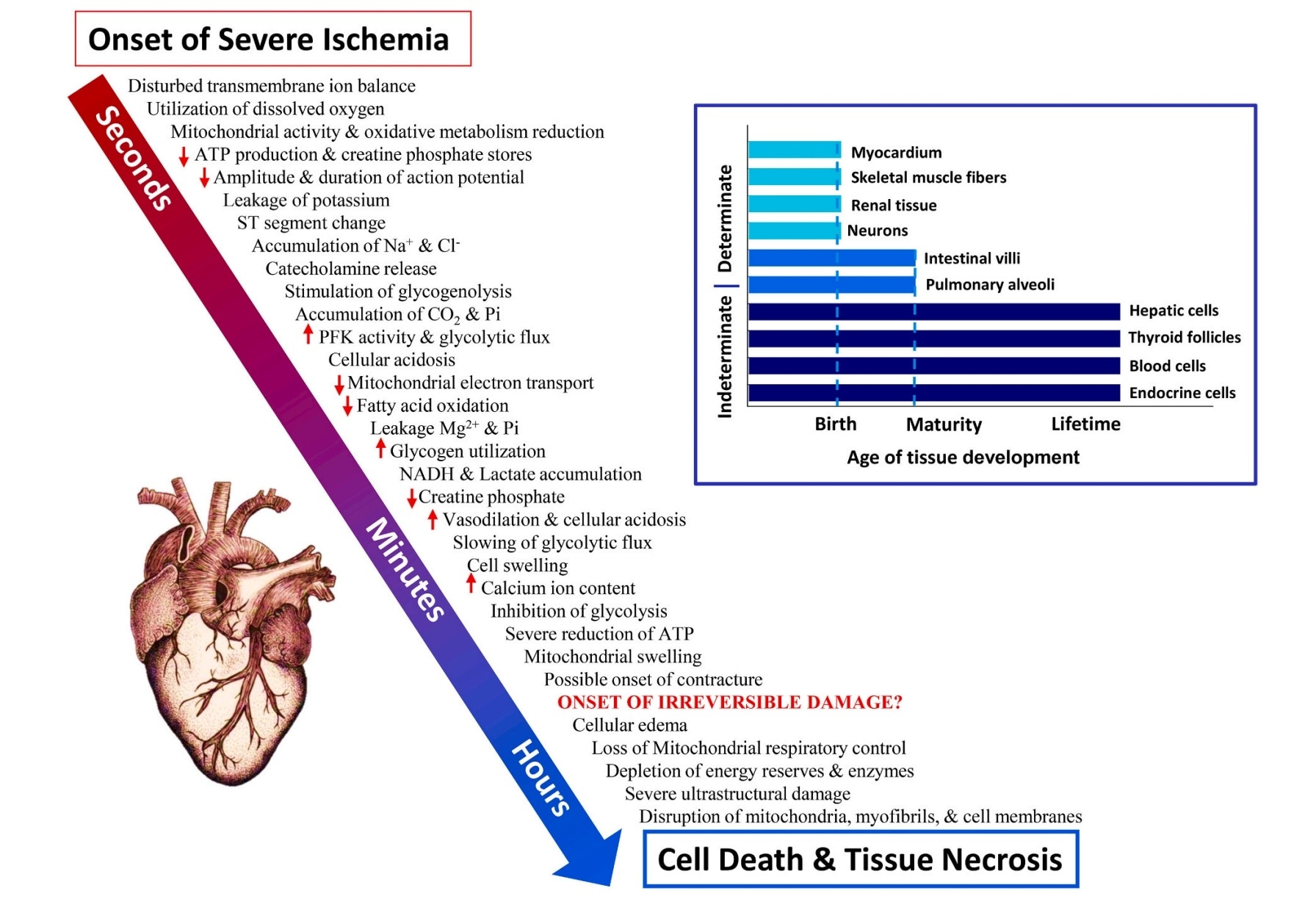
Figure 4 from the review article 'Physiological resiliency in diving mammals: Insights on hypoxia protection using the Krogh principle to understand COVID-19 symptoms'. Image Credit: Williams and Davis (2020)
First, damage to the heart and brain happens very quickly when oxygen is cut off; permanent damage to cells occurs within minutes.
Second, to date, science and doctors cannot make new heart cells or brain cells if they are damaged. That was a wake-up call moment for me regarding COVID-19 infection. Unlike a cold or flu, could this disease, because of its effect on the oxygen pathway, result in permanent organ damage even if the patient survived? Are we as resilient as a diving dolphin or seal? In time, other cells might be able to take up part of the role of the damaged cells, but will 100% function ever be achieved? We are just beginning to see the effects now.
What does your research suggest about COVID-19 patients who are suffering from symptoms long after their initial infection?
Recent studies are now addressing the problems experienced by the “long-haulers”, people that can’t seem to recover from the effects of the original infection. Often it is athletes that are saying that they just cannot seem to return to their original level of training or prowess.
This realization was my second wake-up call moment about the virus. If COVID-19 can create permanent damage along the oxygen pathway leading from the lungs to the heart to an athlete’s muscles, will it compromise elite performance?
For most of us, we just want to be able to run, swim, bike, play basketball, and feel good. For an Olympic or professional sports athlete, the difference between a gold or silver medal or having a championship season is measured on the basis of 1/100th of a second. Will previous COVID infection prove a limiting factor? Just this weekend Keyontae Johnson, a college basketball player for the Florida Gators, collapsed on the court. He is currently in a medically induced coma. His team, family, school and doctors are all wondering if his bout of COVID-19 this summer is a contributing factor. The vulnerabilities to hypoxia we have identified in our cardiac cells may offer clues.
What about the brain and cognitive function; will our ability to get past the “fog” and think creatively or critically be compromised? Years from now, we will probably have answers. But for now, these questions keep me up at night and make me wear a mask.
What important things can the public take from your research?
Obviously there is a lot of discussion about masks, social distancing, lockdowns, and vaccinations these days. It is definitely hard on everyone, especially since no one has all of the answers and everything is happening too fast with this evolving disease.
Given what we do know, the important, conservative thing to do is to stay safe in the best way possible. It would be so regrettable to look back years later and find that an athlete missed their big chance or a promising scientific thinker missed his or her Nobel Prize due to the short- and long-term ravages of this disease.
What are the next steps for your research?
Like August Krogh, I will continue to work with the animals – they have already told me so much about how biology really works.
Where can readers find more information?
Learn more about Terrie's work on her website
Read the full review article here.
About Professor Terrie Williams
Terrie M. Williams is a comparative eco-physiologist with 35 years of research experience concerning the exercise physiology of terrestrial and aquatic mammals such as African lions, sea otters, narwhals, polar bears, and Weddell seals.
As a Professor at the University of California- Santa Cruz, she directs the Integrative and Comparative Energetics (ICE) Lab and the Marine Mammal Physiology Project. Her research expeditions have taken her from the polar regions of the Arctic and Antarctic as well to the savannahs of Africa and the mountainous California coast.
She developed many of the instruments used in her studies including submersible heart rate microprocessors for monitoring the diving responses of dolphins and whales as they feed at sea, and the S.M.A.R.T (Species Movement, Acceleration, and Research Tracking) collar that integrates the energetics and behavior of terrestrial carnivores hunting across diverse landscapes.
Terrie and her students strive to understand the ecological significance of large mammals and the physiological adaptations necessary for species survival in a world that is constantly changing due to human impacts. On her most recent project, she is deploying her heart rate monitors on narwhals and is also measuring their thermal biology using infrared technology. Her primary goal is to understand how the presence of humans may disrupt the normal daily routine of these remarkable deep-diving whales.
Dedicated to solving challenges faced by underrepresented groups in the sciences she is especially interested in introducing field research to students. She has written several popular books, including, The Odyssey of KP2, about her efforts to conserve endangered Hawaiian monk seals which won the 2012 AAAS/Subaru Award for Science Book and Film Prize (Young Adult Science Books).