As the coronavirus disease 2019 (COVID-19) pandemic continues to progress, the first vaccines have been rolled out, and several countries are planning to complete the first round of universal immunization within the first quarter of this year. However, vaccine uptake is a concern that has taken center stage in the recent past, with a flood of misinformation and doubts about the safety and utility of the vaccine spreading far and wide.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Study details
The current study used a cross-sectional design based on an online questionnaire. All participants were above 18 years of age and were working in a healthcare facility of some kind. HCWs were classified into four groups, namely, direct medical provider (DMP), Direct patient care provider (DPCP), Advanced practice providers, and administrative staff who have little direct patient contact.
Attitude of Healthcare Workers toward Vaccines
HCWs were asked about their perception of personal risk of acquiring COVID-19 and whether they had taken care of COVID-19 patients. Moreover, they were asked if they were willing to take the COVID-19 vaccine once available. Possible reasons for not accepting the vaccine were explored as well.
The researchers received approximately 3,500 responses, with over half being below the age of 40 years. Three in four were female, and over 80% were white. Again, 80% had taken a Bachelor’s or higher degree, 44% said they were Democrats, and about 60% denied any comorbidities.
About two-thirds of them were working in an urban healthcare setup, either primary care or subspecialties, with almost 80% being DPCPs. Close to 90% of them felt they were at risk of acquiring COVIDD-19, but only a fifth felt they would develop serious disease symptoms. Less than a tenth were sure they would not get the infection.
Outcomes analysis shows low uptake
Half of the participants reported having taken care of COVID-19 patients, and the same number felt that the vaccine should be left to individual choice.
Only one in three said they would take the vaccine when it became available. About 56% preferred to wait and review safety data before they took the shot. Of this latter group, a tenth each said they would wait for three and six months, respectively, and a fifth said they would wait a year at least. Less than a tenth said they would never take the vaccine ever.
Demographic associations
Significant associations were observed between receiving the vaccine and age, education level, and income stratum. While only a third of HCWs aged 18-30 years were ready to take the vaccine, but almost half of those aged 70 years or above. Only about 30% of females vs. half of male HCWs agreed to take the vaccine and over 40% of non-binary HCWs.
Less than a fifth of black HCWs chose the vaccine, but 44% of Asian HCWs were ready to take the vaccine. Among Native Americans and Hawaiians or Pacific islanders, 80% and 100% were unwilling to take the vaccine without more data to review. A third of Hispanics or Latinos accepted the vaccine.
The lowest willingness to be vaccinated was among HCWs from the West of the country, at 33%. In contrast, those from the South were willing to take the vaccine in approximately half the cases. Only a quarter of those from a rural setting was ready to be vaccinated, but over 40% of Democrats or liberals.
About 22% and 27% of HCWs felt they were immune to the disease and that they would not contract the infection. While willingness to take the vaccine was associated with planning to advise vaccination to friends and family and a higher chance of agreeing that the vaccine should be mandatory, the converse was also true.
Worry about the infection increases vaccine uptake
The analysis by category showed that DMPs were less likely to wait for vaccine reviews, by 53%, compared to HCWs who did not have direct contact with patients. Participants with cancer were also less likely to wait for a review, by over 60%. However, if the subject had already been infected, they were threefold more likely to choose to wait for a review before accepting vaccination. Patients who believed they were immune to COVID-19 due to natural infection were 64% less likely to want to wait for a review.
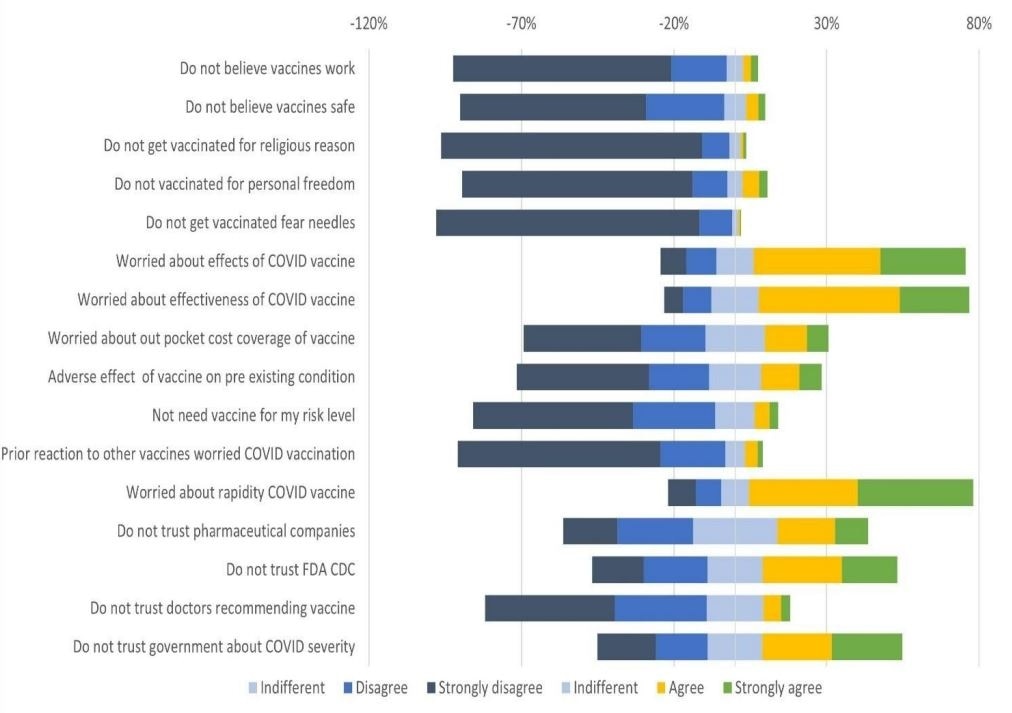
About 90% believed that vaccination, in general, was safe and effective, and neither personal or religious beliefs were quoted in defense of refusing the vaccine. However, ~70% to 75% agreed they were concerned about the safety of the COVID-19 vaccine, its adverse effects, its efficacy, and how rapidly these vaccines were being developed and approved.
While almost three-quarters of HCWs said they did not trust information or interventions by the government, and a half were concerned especially about the reported severity of the disease. A third said they lacked trust that the vaccine development process oversight was properly carried out by regulatory bodies such as the Centers for Disease Control and Prevention (CDC).
In contrast to an earlier study, in April 2020, where over half chose to review their data, only a third were willing to take the vaccine when available. The eagerness to explore literature about the virus is expected of HCWs, and also highlight the importance of publishing peer-reviewed research. It is noteworthy that only 8% refused outright, which indicates that better exposure to scientific data could increase vaccination acceptance significantly. This is supported by the 97% uptake of influenza vaccine in 2020, arguing they were predisposed to consider vaccination a good choice.
What are the implications?
Future actions include targeting subgroups with low acceptance rates, especially those who are already disadvantaged. Further studies are required to explore factors underlying low acceptance of the COVID-19 vaccine.
Interestingly, DPCPs were less likely to accept the vaccine but more likely to be in close and prolonged patient contact, and thus to be at increased risk of being infected with the virus. However, they are also key to the function of the healthcare system. Thus, these HCWs “represent a key subgroup whose health is essential to continue our response to the pandemic.”
As more information comes in about vaccine efficacy and safety, these findings may change. Moreover, a more representative sample may help to minimize bias and to understand the obstacles to greater vaccine uptake.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources