The novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is the pathogen responsible for the ongoing coronavirus disease 2019 (COVID-19) pandemic. Approximately 20-55% of hospitalized COVID-19 patients are reported to have deranged hemostatic laboratory parameters, which suggests coagulopathy.
A better understanding of COVID-19-related coagulopathy is crucial for health care practitioners in order to mitigate the risk of thrombosis and bleeding by tweaking treatment options.
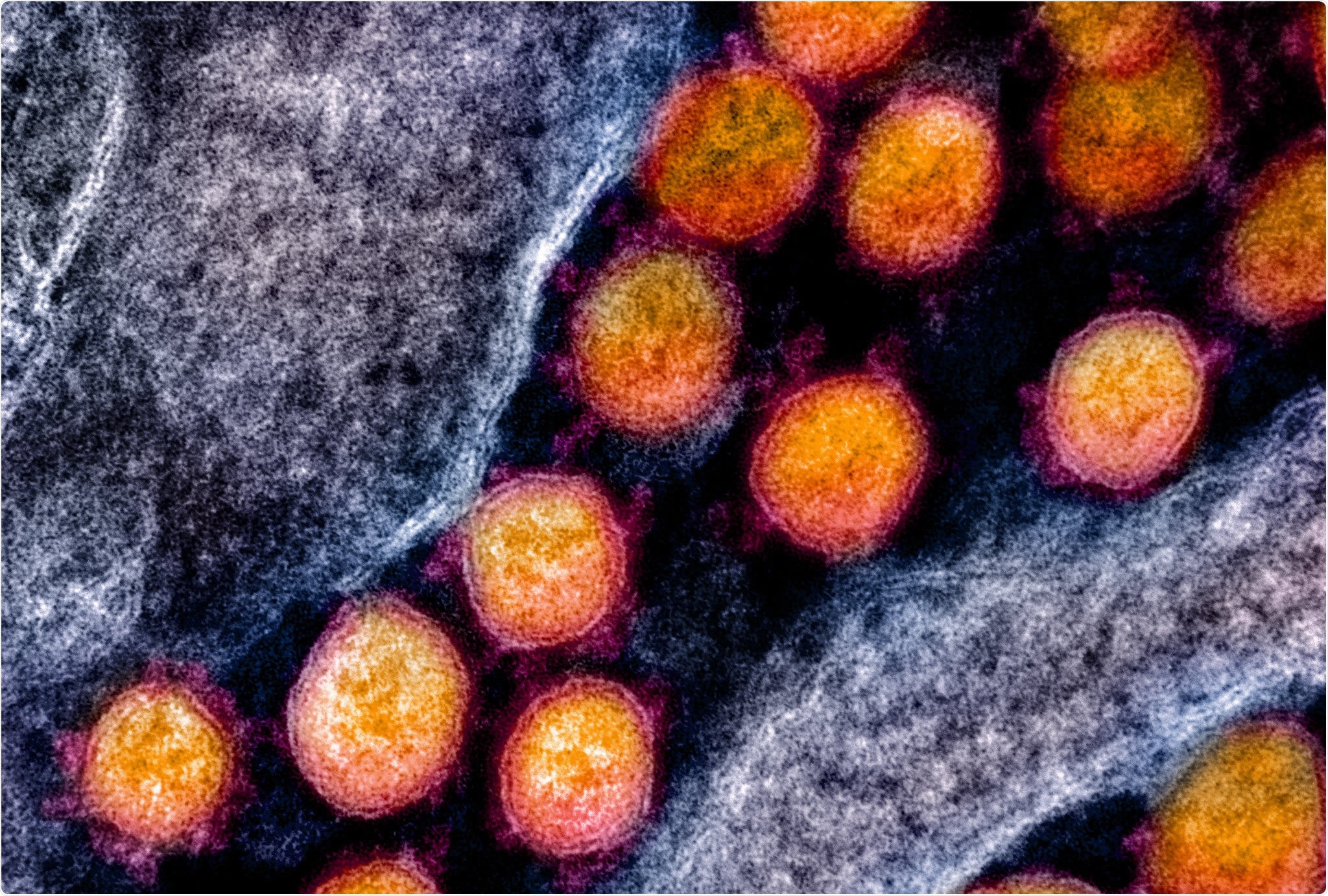
Transmission electron micrograph of SARS-CoV-2 virus particles, isolated from a patient. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Systematic review of the link between hemostatic parameters and poor COVID-19 outcomes
Recently, a team of researchers from Canada and the USA systematically demonstrated the link between hemostatic lab parameters and key clinical outcomes among adult COVID-19 patients. They analyzed hemostatic parameters such as PT and D-dimer concentration in COVID-19 patients and their association with important clinical outcomes such as bleeding, thrombosis, severe disease, and death. The study is published on the preprint server, medRxiv*.
The team performed a systematic review of observational studies, randomized clinical trials, and case series published in PubMed (Medline), CENTRAL, and EMBASE between December 1, 2019, and March 25, 2020. Studies on adult COVID-19 patients that reported at least one hemostatic lab parameter were included in the analysis.
Elevated D-dimer concentration is the strongest predictor of adverse clinical outcomes
The researchers extracted data from 57 studies, including more than 12,000 patients that satisfied their inclusion criteria. 45% of the patients in the studies were women, and the average age of patients was 52 years. Of the studies included in the review, 92.7% (N=38/41) of studies reported an average platelet count greater than 150 x 109/L, 68.2% (N=15/22) of studies reported an average PT of 11 - 14 s, 55% (N=11/20) of studies reported an average activated partial thromboplastin time (aPTT) in the range of
25 - 35 s, and 34.4% (N=11/32) of studies reported a D-dimer concentration above the upper limit of normal (ULN).
Eight studies, including 7 cohorts and 1 case series, reported hemostatic lab values for survivors vs. non-survivors. D-dimer concentrations were reported in 4 studies among non-survivors, and all of them reported an average D-dimer level above the ULN.
Based on the findings, the researchers concluded that most hospitalized COVID-19 patients had a normal platelet count, PT and aPTT values in the upper reference interval, and increased D-dimer concentrations. However, there was no explanation for how these hemostatic parameters were linked to poor outcomes. D-dimer elevation seemed to be the strongest predictor of poor clinical outcomes.
“It has been hypothesized that COVID-19 associated coagulopathy is driven by pulmonary vascular endotheliopathy, which may contribute to the risk of thromboembolism and death in hospitalized patients with COVID-19.”
Findings could help physicians triage severe COVID-19 patients with coagulopathy
The authors believe that these results offer a framework to guide HCPs caring for COVID-19 patients. The results agree with data from hospitalized COVID-19 patients in Wuhan, China, which showed that patients in need of critical care had a median D-dimer concentration of 2.4 mg/L compared to 0.5 mg/L in those who did not require critical care.
Similarly, a New York study reported that 4-times higher D-dimer concentration was associated with about 5-fold higher odds of severe disease compared to a normal D-dimer concentration.
This information can help physicians triage severe COVID-19 patients with coagulopathy and support the recommendation for close monitoring of COVID-19 in-patients with elevated D-dimer concentrations. According to the authors, more studies are essential to confirm this correlation between hemostatic parameters and the risk of adverse clinical outcomes such as bleeding and thrombosis.
“This information will help frontline health practitioners use hemostatic laboratory parameters for prognostication as well as the triage of patients to the appropriate disposition, which is particularly crucial during a pandemic if resources become depleted.”

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
Coronavirus-19 and coagulopathy: A Systematic Review [COVID-COAG], Stephanie G Lee, Michael Fralick, Grace Tang, Brandon Tse, Lisa Baumann Kreuziger, Mary Cushman, Peter Juni, Michelle Sholzberg, medRxiv 2021.01.05.20248202; doi: https://doi.org/10.1101/2021.01.05.20248202, https://www.medrxiv.org/content/10.1101/2021.01.05.20248202v1