Many cases have been reported in which immunocompromised individuals infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have continued to shed the virus for far longer than the typical duration. A new preprint published on the medRxiv* server describes an immunosuppressed patient with coronavirus disease 2019 (COVID-19) who continued to shed the virus for an astounding 154 days. During this period, the virus underwent numerous mutations.
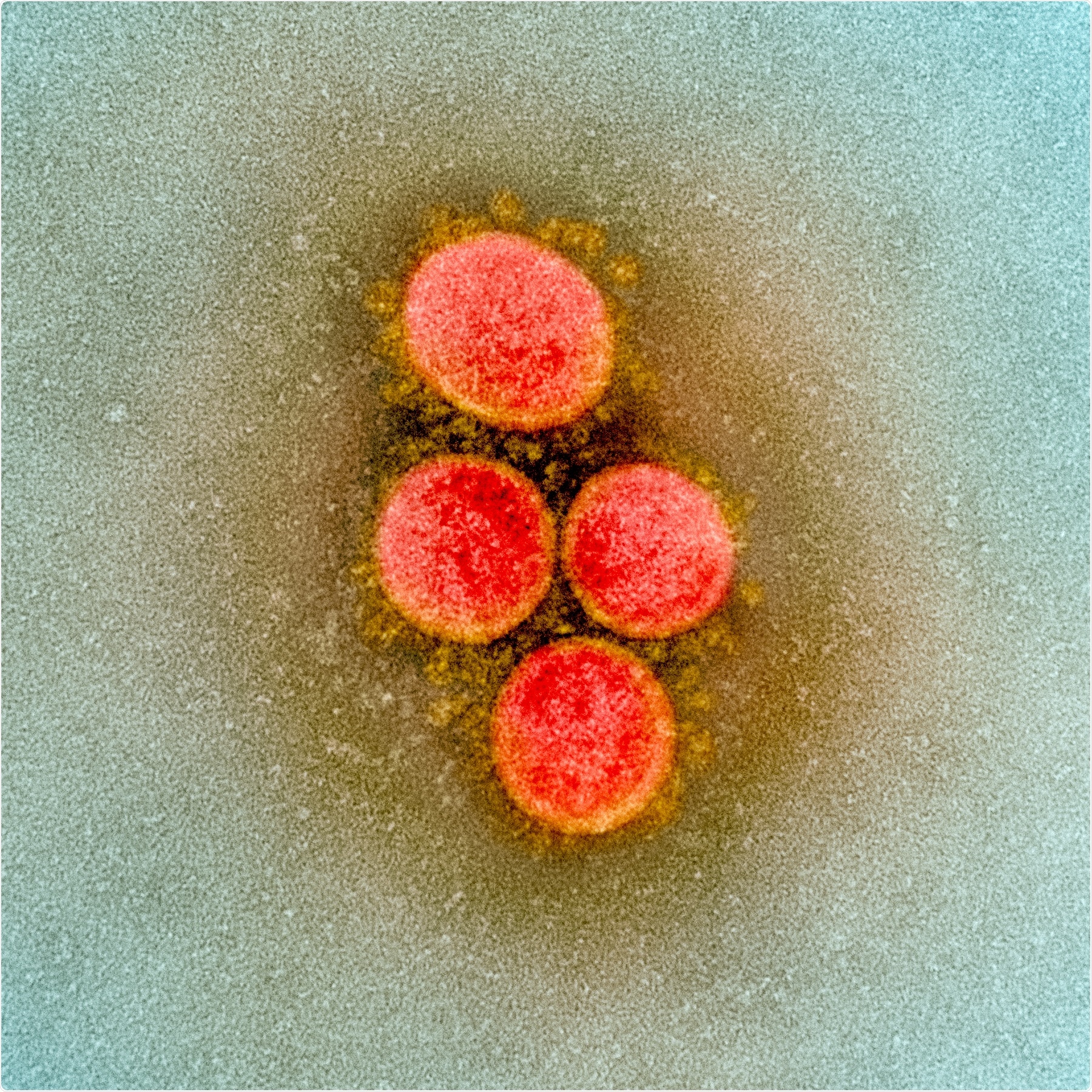
Study: Emergence of multiple SARS-CoV-2 mutations in an immunocompromised host. Image Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
After almost a year of COVID-19, the virus emerged as a new variant, now called the British variant. It is thought that this variant may have higher infectivity and thus greater transmissibility. The sequencing of this variant, which occurred almost immediately, allowed more in-depth research into how the mutations affected the structure of various viral proteins and the molecular determinants of disease transmission. It is thought that genetic diversity arises within a host if the virus is not subject to selection pressure by the host immune response or by therapeutic antibodies.
The current study describes one such patient. The individual was infected for more than 134 days and eventually died of the disease. Throughout the course of the disease, a replicating virus was present in the respiratory tract. The virus also underwent a number of mutations, compared to two other patients who had low B cell counts and most other people with SARS-CoV-2 infection.
The patient was a woman in her seventies who entered hospital with COVID-19 disease, and acute respiratory distress syndrome (ARDS). The symptoms had been present and worsening for two weeks before she was admitted. She was put on high-flow oxygen and later mechanical ventilation. She remained in the intensive care unit until she died, five months after admission.
The patient had a history of follicular lymphoma and had received three cycles of chemotherapy, as well as the anti-CD20 antibody obinituzumab, which depletes B cells. This treatment was stopped just one month before she presented at the hospital. The patient was treated with steroids and convalescent plasma (CP), but not with remdesivir because she also had renal failure.
The samples from the clinical upper and lower respiratory tract contained live replicating virus, with low cycle threshold (Ct) values on reverse transcriptase-polymerase chain reaction (RT PCR), and high viral loads, until she died on day 156 from diagnosis. The first sample collected was on day 20, which the researchers term day 0.
The genome sequence from this patient, as well as two other lymphoma patients with B cell depletion being treated in the same unit at the same time, both of whom had severe COVID-19 over a long period, and also developed ARDS. The latter two patients recovered completely.
The five mutations that defined this patient's strain include D614G, 3037, 14408, and 241, along with deletion at position 28881 of the nucleocapsid antigen. Other unique mutations found in this patient include one seen only in the south of Germany between March 16 and May 11, 2020. In contrast, the other two patients only had the replicating virus for three weeks, at most, with only one or two mutations in 19 days. This is in keeping with the expected number of mutations in this virus. In fact, the index patient also had a similar number of mutations for the first 21 days.
The similarity in the number and pattern of mutations indicates that all three patients were infected from the same source. Detectable mutations dipped by day 30, after two doses of CP, but five new mutations were established at this time and persisted until day 134. Thus, another 11 mutations occurred.
The current patient developed 16 mutations. Typically, the SARS-CoV-2 viruses show 1-2 mutations a month or about 24,000 mutations per genome per year. In the 134 days, the patient's viral genomic samples were analyzed, the expected number of mutations would be 8.6, but instead, there was an unusual number of nonsynonymous mutations, more than three times the number of synonymous mutations.
The patient never developed any detectable specific antibody response to the virus, and the mutations followed the use of CP.
These findings led the researchers to comment, "The therapeutic efficacy of convalescent plasma so far has been disappointing. Its use should be critically evaluated in patients with prolonged viral replication."
This is important in that external pressure from specific antibodies drives selection in a large viral population within an immunosuppressed patient to an unknown extent. This could lead to the emergence of escape mutations and viral variants over time, making it more difficult to control the treatment and containment of the virus.
The researchers also speculate that the mutations in the new variant B1.1.7 may have arisen in a similarly chronically infected patient. Such studies throw light on the ability to trace the course of viral adaptation during chronic infection in order to help understand how host factors influence the viral genome. This would be important in developing both preventive and therapeutic agents.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.