Serum neutralization activity is considered the most important correlate of protection against viral infections after natural exposure to the virus or following vaccination. The same is valid for the severe acute respiratory syndrome virus 2 (SARS-CoV-2), a causative agent of the rampant coronavirus disease (COVID-19) pandemic.
Still, efficacious protection is not reliant only on potency but also on an adequate breadth of serum neutralization due to high-level variation in major antigens of certain viruses. The classic example is the influenza virus, where the lack of breadth hampers the generated antibody response's protective capacity.
Therefore, as many novel SARS-CoV-2 are emerging rapidly worldwide (exemplified by the B.1.1.7, P.1, and 501Y.V2 lineages), it is pivotal to understand whether antibody responses induced by the infection with the virus or by currently available vaccines will also be effective against these new variants.
Consequently, a research group led by Dr. Chloe Rees-Spear from the University College London in the United Kingdom decided to appraise the neutralization of a series of mutated spike glycoprotein SARS-CoV-2 pseudotypes – including the infamous B.1.1.7 variant.
Introducing a myriad of point mutations
In this study, the researchers evaluated the purported role of individual amino acids in enabling the escape from neutralizing antibodies. Initially, a series of point mutations were made to modify the amino acids in SARS-CoV-2 to match those at analogous position in SARS-CoV (i.e., a causative agent of the original SARS outbreak in 2002/2003).
The next step was to emulate individual point mutations that tend to emerge in the real world by generating a pseudotype virus with the use of the B.1.1.7 variant spike sequence. Viral pseudotype mutants were then screened with highly specific assays.
The end-goal was to assess the impact of SARS-CoV spike glycoprotein substitutions on SARS-CoV-2 monoclonal antibody neutralization, as well as to appraise the impact on serum neutralization. Semi-quantitative enzyme-linked immunosorbent assay (ELISA) was one of the main tools in this endeavor.
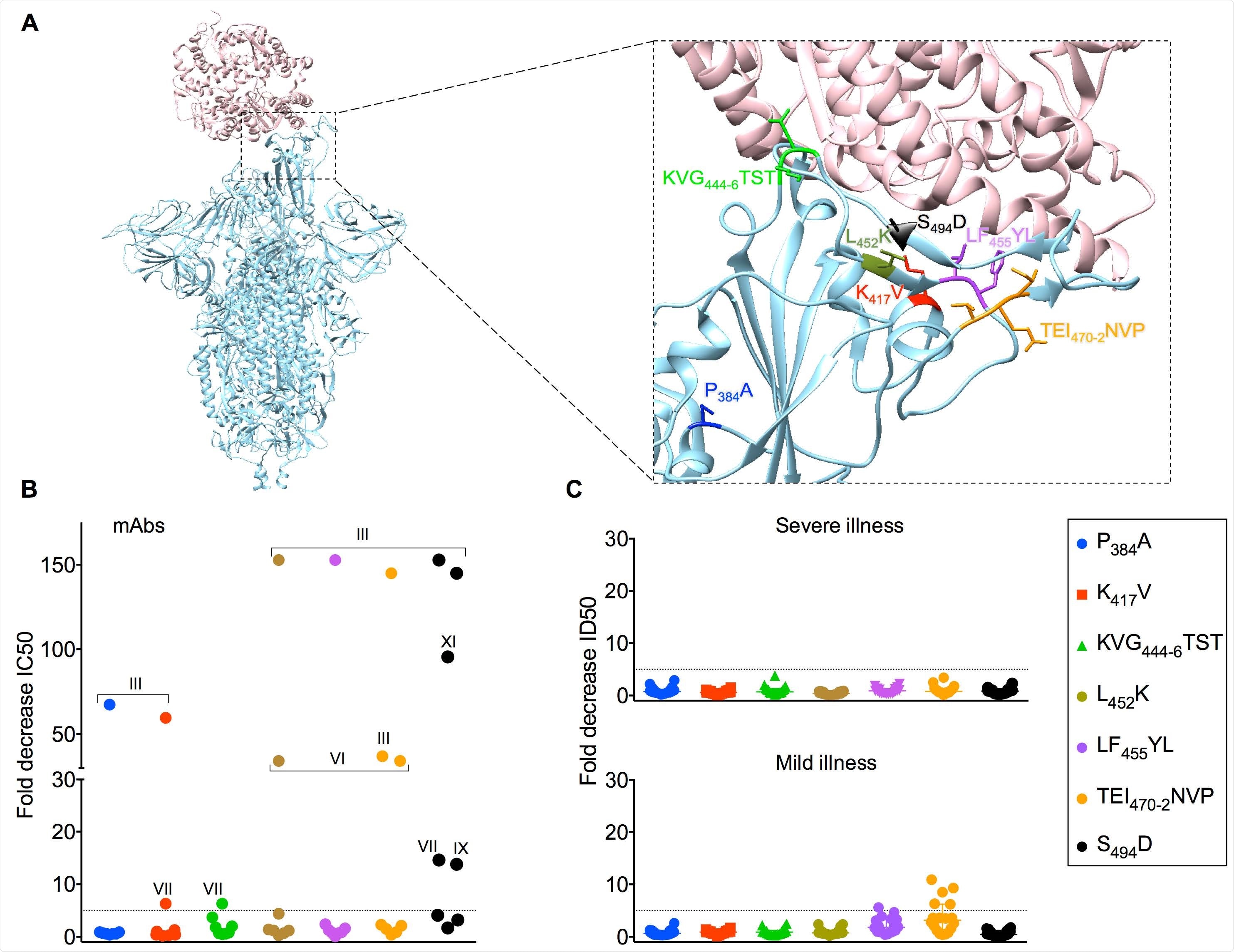
Neutralization by sera is less adversely affected 624 by SARS-CoV amino acid substitutions in SARS-CoV-2 Spike. (A) Representation of SARS CoV-2 Spike trimer (blue) in complex with ACE-2 (pink) (PDB code 7DF4). Magnified image shows mutated amino acid side chains at residues of interest. (B) IC50 values for each mAb against SARS-CoV-2 wildtype pseudotyped virus were divided by the IC50 for each mutant pseudotyped virus against the corresponding mAb to generate the fold decrease in neutralization on the Y-axis. The dotted horizontal line indicates a 5-fold drop in neutralization potency. The competitive binding clusters of each mAb that loses > 5-fold neutralization activity are labeled on the graph. (C) Thirty six serum samples were serially titrated and incubated with the mutant SARS-CoV-2 luciferase-encoding pseudotyped viruses indicated in the legend prior to the addition of HeLa cells expressing ACE-2. After two days, neutralization was measured as the relative reduction in relative light units (RLU) and 50% inhibitory dilution factors calculated using Graphpad Prism. ID50 values for each sera against SARS-CoV-2 wildtype pseudotyped virus were divided by the ID50 for each mutant pseudotyped virus against the corresponding sera to generate the fold decrease in neutralization on the Y-axis. The dotted horizontal line indicates a 5-fold drop in neutralization potency. The 18 serum samples from hospitalized patients are shown in the upper graph labeled “severe illness” and the 18 serum samples from healthcare workers who experience mild/asymptomatic COVID-19 are shown in the lower graph labeled “mild illness”.
Impact on monoclonal antibodies and serum neutralization
In a nutshell, this study has shown that the spike glycoprotein mutations can reduce or eliminate neutralizing activity by individual monoclonal antibodies; on the other hand, serum neutralization was not so strongly affected.
More specifically, only one engineered mutation and none of the perceived spike glycoprotein mutations of the B.1.1.7 variant resulted in an outright escape from neutralizing activity, which was observed for only one out of 36 included serum samples.
"Our results suggest that the majority of vaccine responses should be effective against the B.1.1.7 variant, as the sera evaluated were obtained after infection early in the pandemic when the commonly circulating virus was highly similar in sequence to the vaccines now being deployed", say study authors.
Diminished potency by 5-10 fold was seen in only a small number of samples (i.e., 3 out of 36) interrogated against B.1.1.7 strain; nonetheless, all neutralization titers were still above 1:200 in basically all the cases.
Polyclonal antibody response – a marker of resilience
The most probable explanation of why a greater effect is observed on monoclonal antibodies compared to sera is the intrinsic polyclonality specific for serum neutralization. In other words, when many antibodies target major neutralizing sites in slightly different ways, it is far less sensitive to spike glycoprotein mutations.
"This work highlights that changes in the SARS-CoV-2 spike can alter neutralization sensitivity and underlines the need for effective real-time monitoring of emerging mutations and their impact on vaccine efficacy", explain the authors of this bioRxiv paper.
Likewise, it is also relevant for the potential (and already advocated) use of convalescent plasma, as well as the development of effective therapeutic monoclonal antibodies in our ongoing fight against COVID-19, but also long-term, global management of coronaviruses.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Rees-Spear, C. et al. (2020). The impact of Spike mutations on SARS-CoV-2 neutralization. bioRxiv. https://doi.org/10.1101/2021.01.15.426849, https://www.biorxiv.org/content/10.1101/2021.01.15.426849v1
- Peer reviewed and published scientific report.
Rees-Spear, Chloe, Luke Muir, Sarah A. Griffith, Judith Heaney, Yoann Aldon, Jonne L. Snitselaar, Peter Thomas, et al. 2021. “The Effect of Spike Mutations on SARS-CoV-2 Neutralization.” Cell Reports 34 (12): 108890. https://doi.org/10.1016/j.celrep.2021.108890. https://www.cell.com/cell-reports/fulltext/S2211-1247(21)00204-7.