The coronavirus disease 2019 (COVID-19) outbreak was first detected in Wuhan, China, in December 2019. By March 2020, The World Health Organization declared COVID-19's outbreak a global pandemic. The novel etiological agent of COVID-19, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an infectious and a highly transmissible pathogen. It is transmitted predominantly in the form of aerosols and droplets from an infected person.
The SARS-CoV-2 has infected over 125.6 million individuals and caused over 2.7 million deaths globally. To curb SARS-CoV-2 infection from spreading, and in the absence of a targeted and safe therapeutic drug, non-pharmaceutical interventions have been adopted worldwide. These included lockdowns across states and countries, use of personal protective measures such as masks, frequent hand washing and hygiene maintenance, physical distancing and travel-related measures, such as quarantine, etc.
Even as the pandemic progresses, a 'new normal' has been implemented in many parts of the world, including personal protective behaviors, staggered commuting, physical distancing, and ventilation in offices and commercial facilities. While these measures have helped to limit the spread of SARS-CoV-2, indirect consequences of these lifestyle changes have been observed in many countries.
When 45 out of 50 state governments in the U.S. issued shelter-in-place (SIP) orders from March 19, 2020, to April 6, 2020, to slow the disease progression, a study was conducted to note the effect of the pandemic-related SIP on the bodyweight of people.
Researchers from the University of California, San Francisco, studied the body weight changes of a longitudinal cohort during the initial SIP (shelter-in-place) orders to better understand the possible downstream health implications of a prolonged SIP. They found a significant increase in body weight over the post-SIP period at a rate of roughly a pound and a half weight gain per month following SIP.
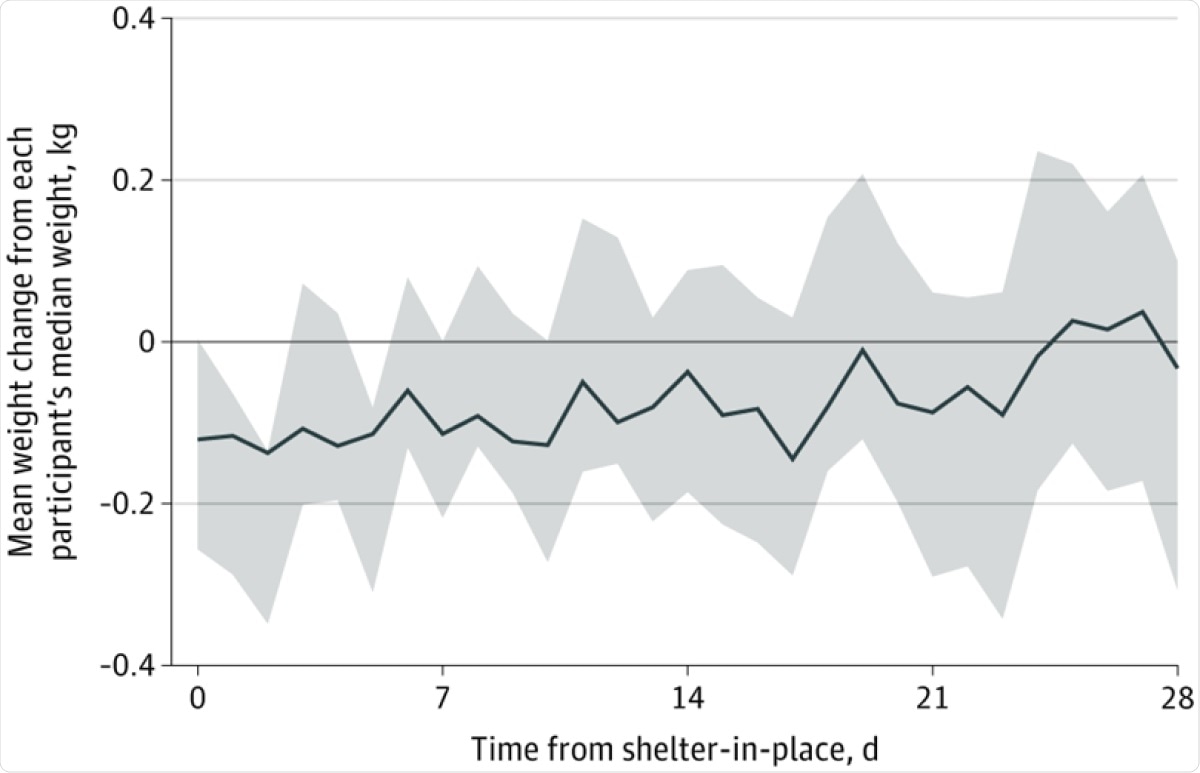
Figure data normalized as weight above or below each participant’s median weight in kilograms. Shaded areas denote the 95% CI for the mean weight of study participants after shelter-in-place.
The researchers emphasized the importance to recognize the unintended health consequences SIP can have on a population level. Their study, which was recently published as a Research Letter, is available in the JAMA Network Open journal.
For this longitudinal analysis, the researchers obtained data from February 1 to June 1, 2020. The study cohort included 269 participants in the Health eHeart Study; they volunteered to report weight measurements from their Bluetooth-connected smart scale (Fitbit [Fitbit Inc] or iHealth [iHealth Labs Inc]).
Although idiosyncratic characteristics of those who happen to own a Bluetooth-connected scale may limit the study's generalizability, following individuals over time to assess their objectively measured weight changes during SIP diminishes threats to internal validity."
The Health eHeart Study is an internet-based longitudinal cardiovascular e-cohort launched on March 8, 2013, and is still ongoing. In this study, the participants contributed at least one weight measurement before, and one measurement after, their state-specific shelter-in-place order was placed.
The researchers obtained all the participants' information – such as the demographic characteristics and medical conditions, race and ethnicity – via online surveys.
The researchers studied the weight change before and after SIP via a linear mixed-effects model with a spline point when SIP orders were issued for each state.
Irrespective of geographic location or comorbidities, the researchers reported that the participants had steady weight gain at a rate of 0.27 kg every ten days; translates into approximately 1.5 lb of weight gain every month.
The researchers warned that although this weight gain may not appear to be clinically important, the prolonged effects might lead to substantial weight gain. The effect of COVID-19 on physical inactivity is a direct consequence on health: an observed decrease in daily step counts, changes in patterns of daily living, and concurrent self-reported increases in snacking and overeating.
The detrimental health outcomes suggested by these data demonstrate a need to identify concurrent strategies to mitigate weight gains, such as encouraging healthy diets and exploring ways to enhance physical activity, as local governments consider new constraints in response to SARS-CoV-2 and potential future pandemics, the researchers write.