The world was hit hard by the COVID-19 pandemic, but New York City was hit the hardest in March 2020. Faced with an unprecedented public health crisis and limited information on the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), strict criteria such as needing to exhibit severe or life-threatening complications made it difficult for many to get a diagnostic test.
Limiting SARS-CoV-2 transmission requires an infected person to quarantine themselves for at least two weeks. New research published on the medRxiv* server highlights the vital role urgent care centers play during the COVID-19 pandemic in New York.
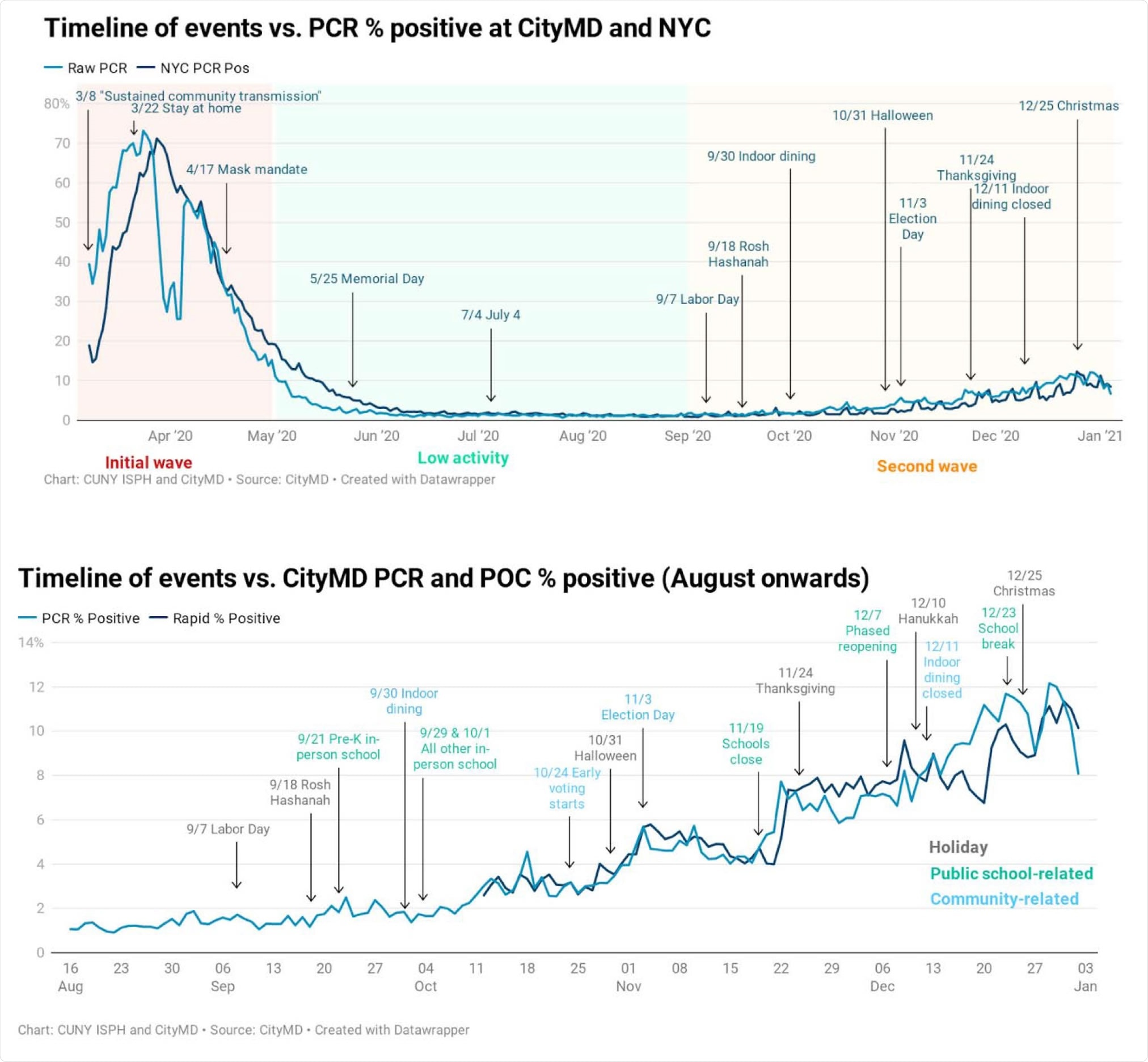
Main events potentially impacting the COVID-19 trends in NYC. Top panel shows PCR percent positivity for PCR tests done at CityMD (light blue) and in NYC (dark blue). The three periods of initial wave, low activity and second wave are shaded in red, blue, and yellow respectively. Bottom panel shows PCR (light blue) and rapid antigen tests (dark blue) positivity rates for CityMD testers focusing on the second wave of the pandemic in NYC. Raw data was used to calculate positivity rates in both plots to be able to visualize the spikes in cases occurring after events that might have facilitated increased in-person contacts. PCR: Polymerase chain reaction. POC: Point-of-care rapid antigen tests.
NYC diagnostic testing results
The researchers performed a retrospective study of coronavirus diagnostic or serologic tests conducted between March 1, 2020, and January 8, 2021. Each person was admitted to at least 1 of 115 CityMD centers in the five boroughs of New York City and surrounding areas in Long Island and Westchester.
A total of 3.4 million individuals received a coronavirus test from CityMD in New York City. Of those, CityMD diagnosed 17% of all cases with testing higher amongst 20-29 years old, non-Hispanic Whites, and females. CityMD performed 43% of PCR tests, 35% of the 15-minute tests, and 22% of serological tests. As the pandemic raged on, serologic testing decreased.
About 88.8% had repeated diagnostic tests on separate days, with most repeated testing between October 2020 and January 2021. Of those, 1.5% had multiple positive tests between the first and last diagnostic test. Only 0.7% of test-takers appeared to be at risk for potential reinfection.
Diagnostic testing increased after incorporating the rapid 15-minute test
Coronavirus testing was high in the last week of April and remained high throughout. Testing was further enhanced after the rapid antigen tests were introduced in October 2020. The researchers note the high positivity rate for SARS-CoV-2 was likely due to heavy restrictions on testing. People who already showed severe infection and got tested were more likely to have a positive test result.
The number of positive tests decreased in late March once New York State mandated lockdown and social distancing guidelines. Until October 2020, there was less than 1% of positive test results. However, positive cases rose once social distancing guidelines gradually lifted with opening up indoor areas again. As a result, the positivity rate increased to about 10% by January 8, 2021.
Minority populations had higher positive test results than White test-takers
Positive SARS-CoV-2 diagnoses were higher amongst minority populations. Hispanics and Native Americans each made up 8% of confirmed cases, 6.4% came from Black people, and non-Hispanic Whites made up 5.4% of cases.
The positive test results decreased in non-Hispanic Blacks and Hispanics in the second wave compared to the first. However, the positivity rate in wave 2 continued to be higher than non-Hispanic White testers.
“Hispanic, non-Hispanic Black and Asian New Yorkers also form a large proportion of essential workers and healthcare workers, further increasing their risk of infection with SARS-CoV-2. It is possible that due to the nature and hours of essential work, there are fewer opportunities and free time to test, making it more likely to test only when symptomatic or after a known exposure, resulting in a higher individual and test-level prevalence.”
Manhattan had the lowest number of positive test results compared to other boroughs and surrounding New York City areas.
Seropositivity rates
Overall seropositivity was 21.6% in 693,205 people given at least one antibody test. Children from ages 5-9 and 10-14 had high seropositivity at 26.9% and 27.3%, respectively. Seropositivity was higher with non-Hispanic Blacks at 25.4%, Hispanics at 30.6%, and Native Americans at 24.4%.
New York City boroughs Bronx and Queens have a high minority population, and the high seropositivity amongst residents coincided with other demographic results. Bronx residents had a 31.2% seropositivity, and Queens residents had a 30.5% seropositivity compared to the 17% seropositivity observed in Manhattan.
“Because people of color are more likely to reside in New York neighborhoods that also have higher concentrations of essential workers, and higher levels of household crowding, the virus could have spread more rapidly in these communities early in the pandemic,” wrote the authors.
Important Notice
*medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.