Among the major risk factors for complicated coronavirus disease (COVID-19) caused by SARS-CoV-2, adiposity and excess visceral fat are certainly those that endanger the infected individuals. Other important ones are diabetes, high blood pressure (hypertension), chronic lung disease, and smoking.
There are also issues with the correlations of immune protection in individuals with the risks mentioned above, especially central obesity. Thus, even before vaccines were on the market, there were grave concerns that their presence may result in lower protection.
A recent study has shown that a higher body mass index (BMI) is associated with lower serological responses after the COVID-19 vaccine in Italian healthcare workers. Likewise, hypertension and inadequate response to vaccines may have roots in the dysfunctional immune system, at least according to some recent research evidence.
In order to explore variables associated with the serological response after Pfizer/BioNTech COVID-19 mRNA vaccine in more depth, a research group led by Dr. Mikiko Watanabe from the Sapienza University of Rome in Italy conducted a comprehensive, single-center observational study.
From laboratory assays to imaging methods
In this study, a total of 86 healthcare workers that underwent vaccination against COVID-19 were enrolled in January and February 2021. All subjects were given two COVID-19 mRNA vaccine inoculations (Pfizer/BioNTech) three weeks apart.
Consequently, blood samples were taken for the analysis before the first shot and one to four weeks after the second shot. Antibodies against SARS-CoV-2 were measured by using a commercially available sandwich electrochemiluminescence assay.
Clinical history, demographic data, and vaccine side effects were recorded. Moreover, anthropometric parameters were measured at baseline, while body composition measurement has been performed using dual-energy X-ray absorptiometry.
Blunted production of antibodies
This study has shown that patients with central obesity had lower titers of SARS-CoV-2 antibodies in comparison to those without central obesity; furthermore, smokers exhibited a blunted immune response when compared to non-smokers, which was also the case when comparing individuals with increased blood pressure or lipids to those with normal levels.
A detailed analysis has also shown that higher circumference of the waist, smoking, increased blood pressure, and longer time since second vaccine dose was linked to lower titers of antibodies – Independent of body mass index, gender and/or age.
Nonetheless, the link between waist circumference and antibody titers was not demonstrated when controlling for body fat, pointing towards visceral accumulation as a potential explanation. Interestingly, eventual side effects after the first or second dose of the vaccine were not related to different antibody titers, and neither was influenza vaccination in the preceding 12 months.
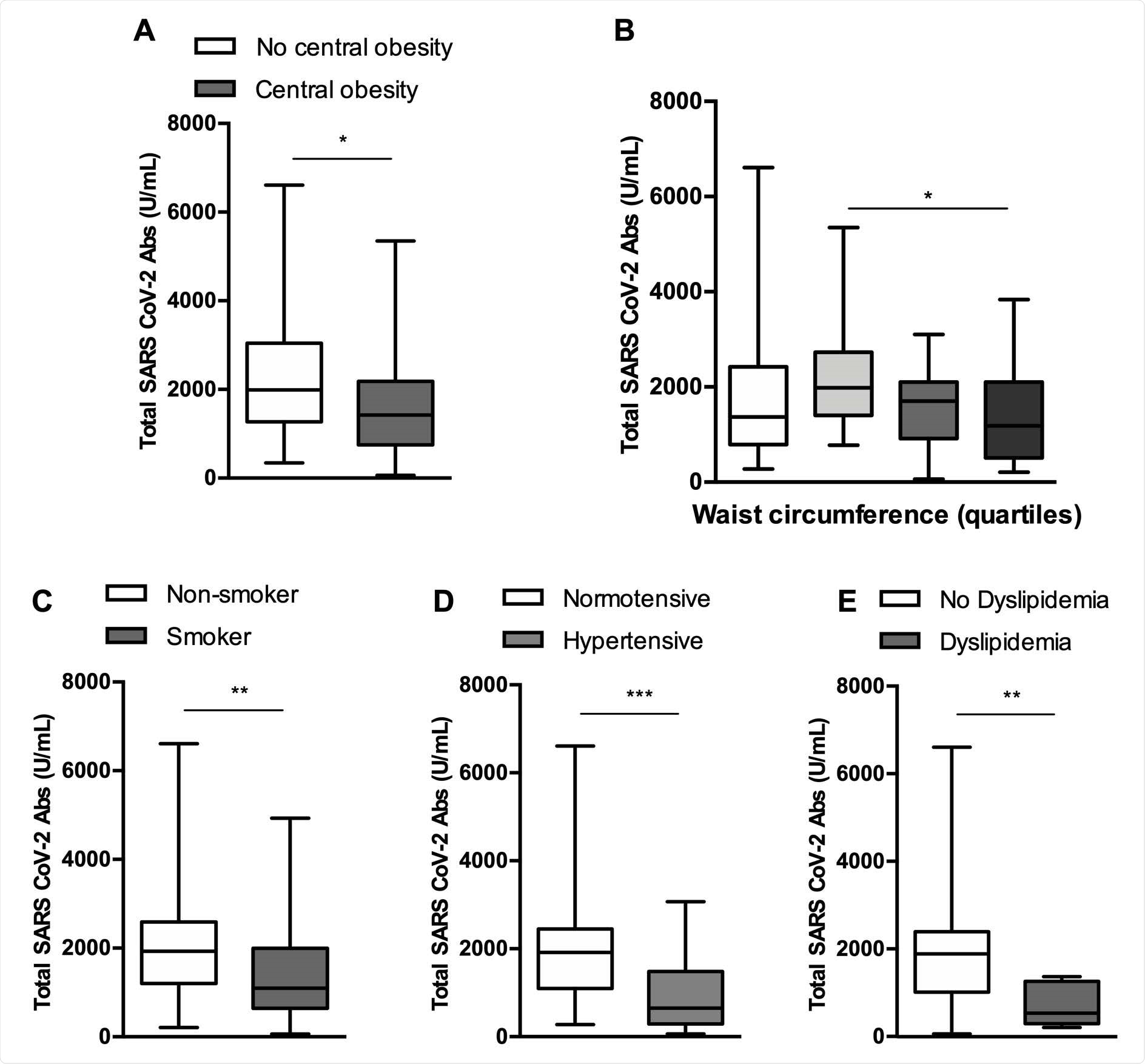
Serological response of analyzed subpopulations. Anti SARS CoV-2 Antibody titers were significantly lower in subjects with central obesity (A), subjects belonging to the second quartile of waist circumference compared to those belonging to the fourth quartile (overall p= .046) (B), smokers (C), hypertensive subjects (D), dyslipidemic subjects (E). *p<.05, **p<.01, **p<.001, ***p<.000
Shifting the optimal vaccine schedule?
Although it is currently impossible to appraise whether a lower amount of SARS-CoV-2 antibodies leads to a higher likelihood of developing COVID-19, previous experience teaches us that this may well be the case; hence, all factors above linked with a blunted immune response warrant further scrutiny.
“The fact that the antibody response is blunted in certain subjects shortly after the second inoculation must lead to a highly vigilant approach, as medium and long-term data will become available only when the schedule will have been necessarily set already”, caution study authors in this medRxiv paper.
This means that smokers and individuals with central obesity and/or hypertension could benefit from earlier vaccine boosters or different vaccine schedules, which is why further research endeavors on schedule adjustments should be conducted.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Watanabe, M. et al. (2021). Central obesity, smoking habit and hypertension are associated with a blunted serological response to COVID-19 mRNA vaccine. medRxiv. https://doi.org/10.1101/2021.04.13.21255402, https://www.medrxiv.org/content/10.1101/2021.04.13.21255402v1
- Peer reviewed and published scientific report.
Watanabe, Mikiko, Angela Balena, Dario Tuccinardi, Rossella Tozzi, Renata Risi, Davide Masi, Alessandra Caputi, et al. 2021. “Central Obesity, Smoking Habit, and Hypertension Are Associated with Lower Antibody Titres in Response to COVID‐19 MRNA Vaccine.” Diabetes/Metabolism Research and Reviews, May. https://doi.org/10.1002/dmrr.3465. https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3465.