Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus responsible for the outbreak of the COVID-19 disease. The virus emerged in China in late 2019, with viral transmission reaching pandemic proportions in early 2020. The average mortality rate of COVID-19 is under 2%, as this virus also causes asymptomatic infections in a large proportion of the population. However, in a small percentage of infected individuals, the virus causes symptomatic infections, leading to severe disease, hospitalizations, and deaths. There are also reports of persistent symptoms and long-term sequelae post recovery from COVID-19, which indicates a potentially more profound health crisis.
Containment strategies and lockdowns slow down the transmission of the virus and allow time to prepare a public health strategy, devise treatments, and develop vaccines without overwhelming the healthcare system. Although achieving herd immunity via mass vaccination will help eradicate the virus, there needs to be concerted coordination globally to significantly reduce transmission rates before the virus mutates into newer and more infectious variants that no longer respond to available vaccines.
This is a considerable challenge because the virus is currently infecting the global population at a high rate, providing ideal conditions for mutation. Hence there is a possibility that the disease may remain a health crisis for the foreseeable future. This makes it a priority to gain clear insights into the factors responsible for COVID-19 disease progression, which could help improve disease management and develop better treatment options.
The key symptoms of COVID-19 include cough, fever, and fatigue, with some people experiencing anosmia and a loss of taste. In people experiencing severe COVID-19, lung capacity decreases considerably and oxygen levels in the blood drop dangerously low, requiring supply of nasal oxygen and intubation using ventilators in very severe cases. The reasons behind the spectrum of differences in disease severity across the population and why COVID-19 affects the elderly population and those with comorbidities more severely are unclear.
.jpg)
Atomistic reconstruction of the glycosylated spike of SARS-CoV-2 interacting with its glycosylated receptor ACE2. The interaction between a spike in open conformation and ACE2 is represented. The binding domains in the spike and ACE2 involved in the interaction are colored in green and blue respectively. Note that not all glycans are present on the open spike (see Methods for details).

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Machine learning models to help mine scientific papers in the CORD-19 database
Researchers from Switzerland recently developed machine learning models to help mine 240,000 scientific papers in the CORD-19 database. Using the models, they constructed knowledge graphs to analyze the extracted data and search for a potential reason for disease severity. The study is published on the preprint server, medRxiv*.
The literature analysis pointed to elevated blood glucose levels as a leading facilitator in the progression of COVID-19. Evidence linking elevated glucose to various steps in the life cycle of the virus and presentation of COVID-19 symptoms were also found.
The observations suggested that blood glucose elevation provided ideal conditions for SARS-CoV-2 to attack the lung’s immune defense system and gain access to alveolar cells before binding to the human ACE2 receptor. High glucose levels also enabled the entry of the virus to the pulmonary cells and rapid viral replication within cells and induced a pulmonary inflammatory response. This massive immune response overwhelms an already weakened immune system and triggers a series of events causing systemic inflammation, cell damage, and the release of cytokines.
The researchers analyzed data across the papers, reconstructed the virus at the pulmonary airway surface, and then performed quantitative computational modeling of the impact of glucose levels on the infection process. They concluded that glucose level elevation could facilitate COVID-19 progression through multiple mechanisms. This explains the variation in disease severity across the population.
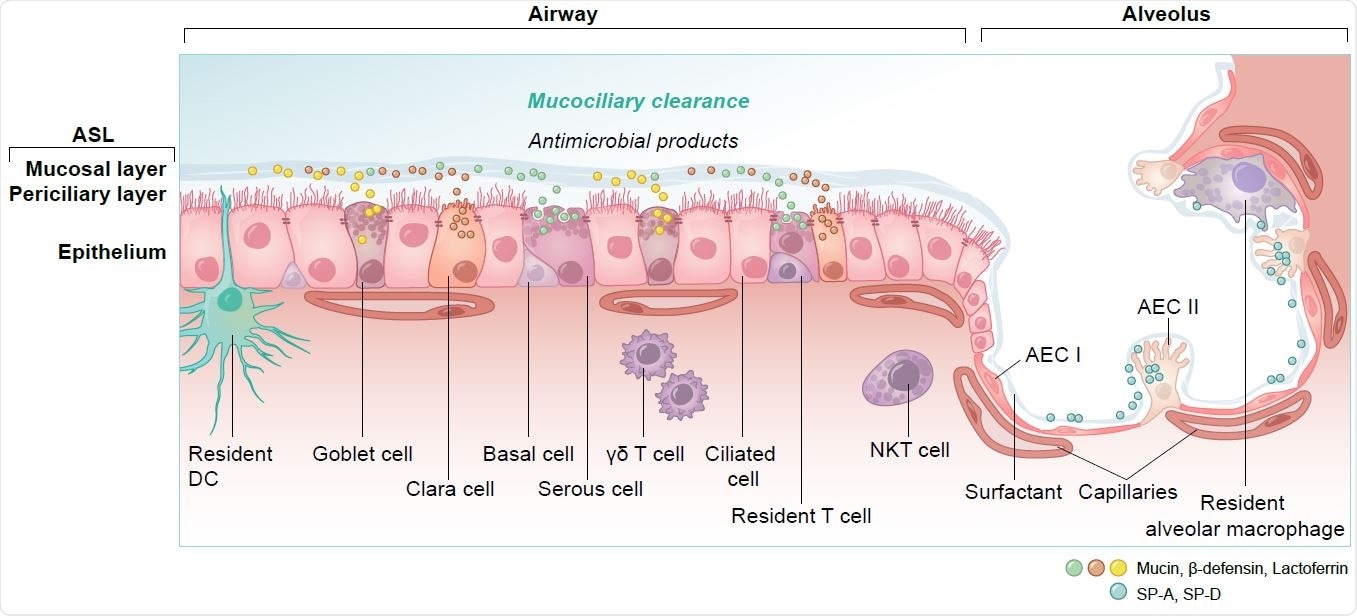
Overview of cell types and innate immunity in the epithelium of the lung. DC = dendritic cell, NKT = natural killer T cell, γδ T = gamma delta T cell, AEC I and AEC II = alveolar epithelial cells, SP-A, SP-D = surfactant protein A and D.
Summary of the findings
To summarize, the findings suggest that patients with severe COVID-19 usually present with elevated blood glucose levels, which impact several biochemical pathways that facilitate various steps in SARS-CoV-2 infection. Elevated blood glucose increases the amount of glucose in the pulmonary airway surface liquid (ASL), which destroys the primary antiviral defenses of the lungs and enables viral infection and replication.
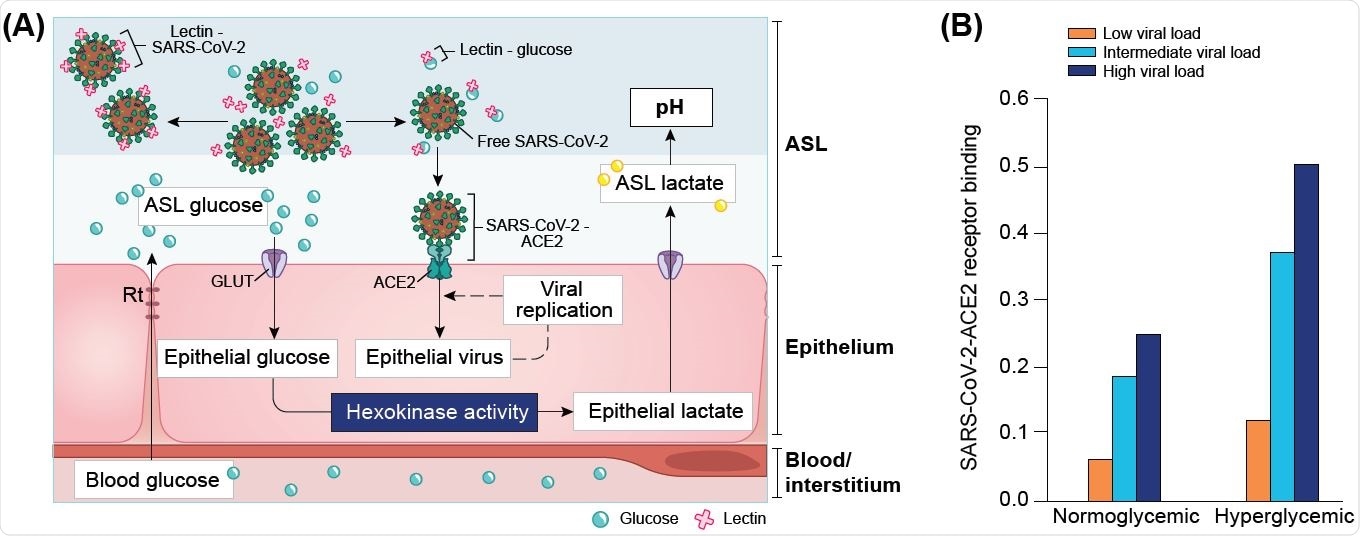
Computational modeling of glucose-dependent SARS-CoV-2 infection. (A) Schematic representation of the parameters used in the different SARS-CoV-2 primary infection computational models. GLUT = Glucose transporters (1, 2, 10); Rt = paracellular resistivity (1/Rt = paracellular conductivity in model) (see methods for details). (B) Simplified modeling of SARS-CoV-2 - ACE2 binding in a normoglycemic or hyperglycemic patient, as a function of the viral load (represented by three different viral contents at the time of infection, see Definition of viral loads in methods). Normoglycemic = 0.4 mM ASL glucose, hyperglycemic = 1.2 mM ASL glucose.
Elevated glucose levels cause dysregulation of the immune response resulting in a cytokine storm and acute respiratory distress syndrome. Elevated glucose levels also work synergistically with the virus-dependent inactivation of ACE2 to rapidly escalate the disease to thrombotic events and multi-organ failure.
“The study proposes diagnostic recommendations, new areas of research and potential treatments, and cautions on treatment strategies and critical care conditions that induce elevations in blood glucose levels.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Elevated Blood Glucose Levels as a Primary Risk Factor for the Severity of COVID-19, Emmanuelle Logette, Charlotte Lorin, Cyrille Favreau, Eugenia Oshurko, Jay S. Coggan, Francesco Casalegno, Mohameth François Sy, Caitlin Monney, Marine Bertschy, Emilie Delattre, Pierre-Alexandre Fonta, Jan Krepl, Stanislav Schmidt, Daniel Keller, Samuel Kerrien, Enrico Scantamburlo, Anna-Kristin Kaufmann, Henry Markram, medRxiv, 2021.04.29.21256294; doi: https://doi.org/10.1101/2021.04.29.21256294, https://www.medrxiv.org/content/10.1101/2021.04.29.21256294v1
- Peer reviewed and published scientific report.
Logette, Emmanuelle, Charlotte Lorin, Cyrille Favreau, Eugenia Oshurko, Jay S. Coggan, Francesco Casalegno, Mohameth François Sy, et al. 2021. “A Machine-Generated View of the Role of Blood Glucose Levels in the Severity of COVID-19.” Frontiers in Public Health 0. https://doi.org/10.3389/fpubh.2021.695139. https://www.frontiersin.org/articles/10.3389/fpubh.2021.695139/full.