Although extensive studies have been carried out on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and evidence exists that pregnant women are at elevated risk of severe COVID-19, the impact of maternal infection on the fetus is not clear. The majority of pregnant women infected with SARS-CoV-2 are asymptomatic or experience mild symptoms.
However, some pregnant women in the third trimester with SARS-CoV-2 infection seem to be at increased risk of requiring hospitalization and ICU admission. The rates of maternal SARS-CoV-2 infection also increased during the second wave of the pandemic. A national UK surveillance study reported that neonatal SARS-CoV-2 infection is not common even in infants born to mothers with perinatal SARS-CoV-2 infection.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Studying the potential impact of SARS-CoV-2 exposure in utero on the neonate
Recently researchers determined the immunological status of infants born to mothers who had confirmed SARS-CoV-2 infection during pregnancy. Their objective was to determine the potential impact of SARS-CoV-2 exposure in utero on the neonate. This study is published on the preprint server, bioRxiv.*
The findings showed no evidence of vertical SARS-CoV-2 transmission, but it was clear that maternal SARS-CoV-2 specific Immunoglobulin G (IgG) was transferred to infants, to a lesser extent in active or recent maternal infection cases. Babies born to mothers with recent or ongoing SARS-CoV-2 infection had increased circulating pro-inflammatory cytokines and elevated percentages of innate immune cells compared to babies born to uninfected mothers.
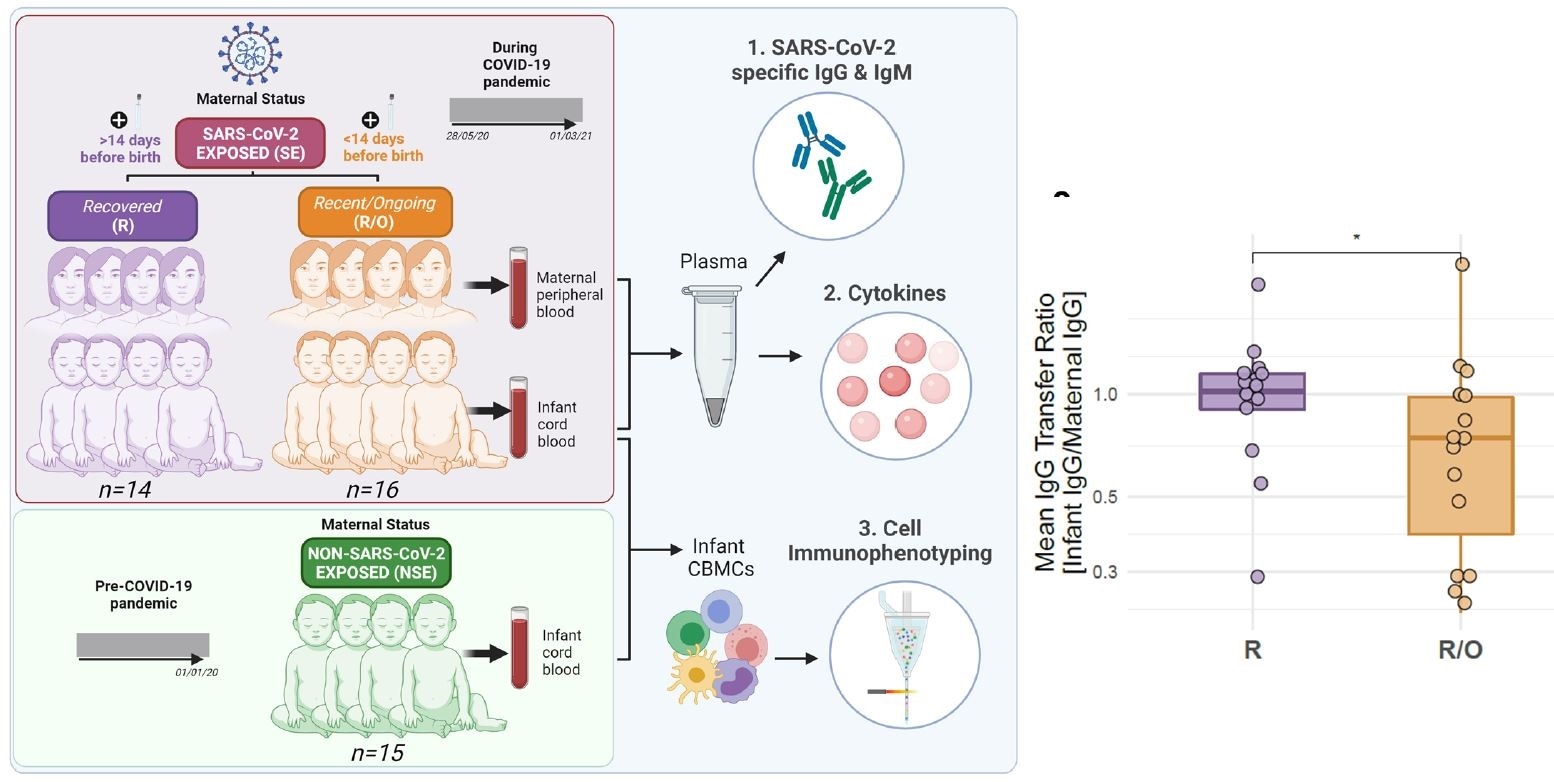
Infants born to SARS-CoV-2 exposed mothers are IgG+IgM- and reduced antibody transfer is seen in the recent/ongoing group. a, Study outline illustrating recruitment of infants and mothers in the SE group (n=30), comprised of two groups (R: n=14, R/O: n=16), and infants in the NSE group (n=15). Figure created with BioRender.com.
Results show that maternal SARS-CoV-2 specific IgG is transferred to infants born to mothers with perinatal SARS-CoV-2 infection
Also, greater frequencies of FOXP3+ regulatory T cells and circulating IL-10 showed the mechanism behind the neonatal effector response. Moreover, infants born to mothers who were exposed to SARS-CoV-2 during pregnancy had enhanced cytokine functionality. This shows that maternal SARS-CoV-2 infection influences in utero priming of the fetal immune system.
“Our study adds further evidence suggesting the 2nd trimester may represent more opportune vaccination timing, at least with respect to the transfer of passive immunity to the infant.”
According to the authors, the study offers a comprehensive immune map of neonates born to mothers with SARS-CoV-2 exposure during pregnancy. While the study did not observe vertical SARS-CoV-2 transmission, it did find multiple immunological alarms in the infants associated with maternal SARS-CoV-2 infection during pregnancy, especially with recent or ongoing infections.
Transfer of maternal SARS-CoV-2-specific IgG to the neonates suggests transfer of protective immunity
Overall, the findings of this study suggest an immunological imprint on the neonate following maternal SARS-CoV-2 infection, with potential long-term consequences. In utero exposure to environmental factors, pathogens, and/or maternal inflammation have been shown to affect the developing immune system of the fetus and the subsequent responses to infection and immune-mediated diseases, and neurodevelopmental problems. The transfer of maternal SARS-CoV-2 IgG to the fetus suggests the transfer of protective immunity to infants.
“Neonatal immune profiling following vaccination in pregnancy may also determine what level of maternal immune activation drives the neonatal imprinting observed.”
Observations from this study may influence COVID-19 vaccination regimen for pregnant women
The researchers feel that based on the observations in survivors of in utero exposure to the 1918 Spanish influenza pandemic, long-term effects on infants cannot be ruled out. It is currently unclear if antibodies induced via vaccination vs. natural infection differ in their glycosylation status and placental transfer.
SARS-CoV-2 vaccination in the second and third trimesters induced placental transfer of antibodies, but with a reduced transfer ratio in the last trimester. The data from this study may also influence the COVID-19 vaccination regimen for pregnant women. The authors believe that long-term follow-up of the infants who were part of this study will help establish if maternal SARS-CoV-2 exposure has a lasting impact on the infants.
“More data are needed to establish if these changes specifically relate to enhanced protection from SARS-CoV-2 mediated disease or are detrimental if the infant is born in a milieu of inflammatory cytokines.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
The legacy of maternal SARS-CoV-2 infection on the immunology of the neonate Sarah Gee, Manju Chandiramani, Jeffrey Seow, Carlotta Modestini, Abhishek Das, Katie J Doores, Rachel M Tribe, Deena L Gibbons doi: https://doi.org/10.1101/2021.05.27.446014, https://www.biorxiv.org/content/10.1101/2021.05.27.446014v1
- Peer reviewed and published scientific report.
Gee, Sarah, Manju Chandiramani, Jeffrey Seow, Emily Pollock, Carlotta Modestini, Abhishek Das, Timothy Tree, Katie J. Doores, Rachel M. Tribe, and Deena L. Gibbons. 2021. “The Legacy of Maternal SARS-CoV-2 Infection on the Immunology of the Neonate.” Nature Immunology, October. https://doi.org/10.1038/s41590-021-01049-2. https://www.nature.com/articles/s41590-021-01049-2.