I am a Professor of Vascular Biology at the University of Leeds and have been researching the field of thrombosis and hemostasis for more than 30 years.
One question I have wanted to answer for some time is: Why do certain clots embolise and cause pulmonary embolism (clots in the lungs) and others do not? Also, I wanted to know what, if anything, crosslinking of the building material of the clot (a protein called fibrin) by a transglutaminase enzyme called factor XIII had to do with this.
Blood clots in the lungs kill more than two thousand people each year in the UK alone yet how they form is still largely unknown until now. Why was this?
We knew that clots in the lungs can arise from clots in the deep veins of the legs or arms, by breaking off from the site of thrombosis in the limbs, and then traveling in the bloodstream to the lungs to block a vessel there and cause difficulties in breathing.
However, we did not know why certain clots break off and do this, while others do not.
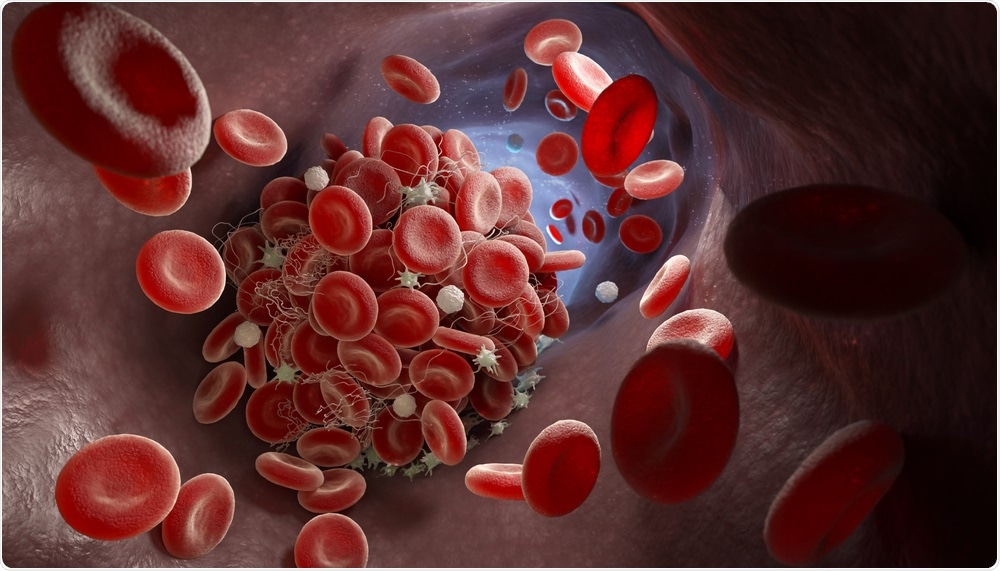
Blood Clot. Image Credit: Tatiana Shepeleva/Shutterstock.com
What role does deep vein thrombosis play in blood clot formation?
Deep vein thrombosis occurs when a blood clot forms in the large veins of the arm or leg. Veins are blood vessels that have valves to make sure the blood flows against the direction of gravity. Usually, the clot formation starts around the valves in these veins.
A combination of factors can contribute to clot formation, including prolonged immobility, endothelial cell (cells that line the blood vessel) dysfunction, and a procoagulant state (heightened blood clotting activity) due to genetic or environmental factors.
Can you describe how you carried out your latest research into blood clots?
First, we made a new model in which particular crosslinks induced by factor XIII do not occur since we genetically mutated the crosslinking sites. Then we developed a new model of pulmonary embolism using powerful new imaging methods to analyze embolization of the clots to the lungs.
We also used nanotechnology called atomic force microscopy to test the strength of individual fibrin fibers.
What did you discover? What role does the protein fibrin play in blood clots?
We found that when particular crosslinks induced into fibrin by factor XIII called gamma chain crosslinks do not occur, individual fibrin fibers are broken much more easily and at lower levels of stretch. Then we found that in the absence of these crosslinks, clots that form in the vena cava (central vein) break off much more easily and generate more emboli in the lungs.
The differences we observed were substantial, with an approximately 40% increase in lung emboli.
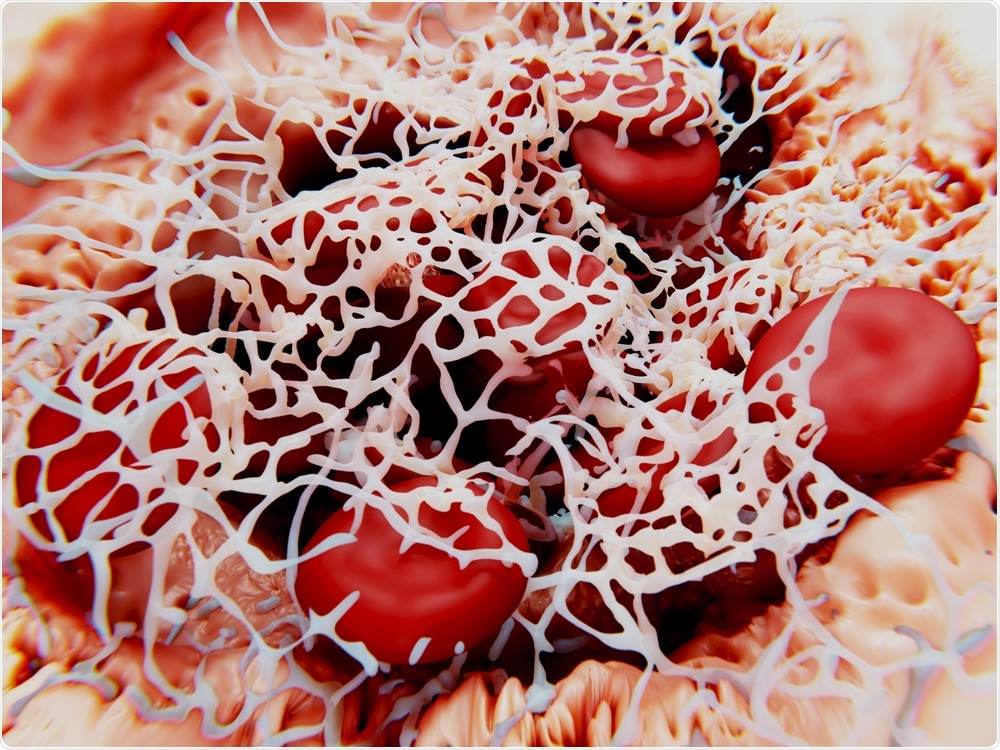
Fibrin. Image Credit: Juan Gaertner/Shutterstock.com
Why is research into blood clots of particular importance currently in light of the ongoing COVID-19 pandemic?
We know that patients with severe COVID-19 have a really high risk of thrombosis, with a particularly high risk of clots in the lungs.
If we can reduce pulmonary embolism, this may also greatly help patients with COVID-19.
How will your research help to identify new drugs that can target blood clots?
Now that we know the molecular mechanism that helps to prevent pulmonary embolism, we can make sure that this mechanism remains fully functional when we try to treat the clots with new anticoagulants or new clot-busting drugs called thrombolytics.
Do you believe that with continued research into blood clot formation we will be able to reduce the number of people dying from them each year?
I am convinced we can achieve this. Blood clots are a leading cause of death and debilitating disease worldwide.
We are now in a unique position to develop new drugs that prevent clots or break them down that can replace currently used drugs, which are not always effective and can cause a heightened risk of bleeding. Newer medications to be developed will be more effective and cause fewer side effects including bleeding.
What are the next steps in your research?
We are having clear ideas of which process we need to target to reduce thrombosis while avoiding deadly emboli.
Our next steps will be to generate candidate drugs to be tested in our models of thrombosis and thromboembolism.
Where can readers find more information?
About Professor Robert Ariëns
Robert Ariëns is a Professor of Vascular Biology, Wellcome Trust Investigator, and Head of the Department of Discovery and Translational Science, Leeds Institute of Cardiovascular and Metabolic Medicine at the University of Leeds.
Ariëns obtained a BSc in Biology from the University of Utrecht in 1990, and a Ph.D. from the University of Maastricht in 1997. He was President of the British Society for Haemostasis and Thrombosis (2016-2018) and President of the International Fibrinogen Research Society (2014-2018). He is a member of the JTH Editorial Board, and holder of a Hemker Visiting Chair, University of Maastricht.
Ariëns was awarded the Outstanding Investigator Award by the International Fibrinogen Research Society, July 2012, and was Chair of the Factor XIII and Fibrinogen ISTH Subcommittee from 2002-2006. Research of the Ariëns laboratory has a strong focus on mechanisms in thrombosis and hemostasis, with a particular interest in clot structure and function.
He has published extensively in the most influential journals of the field including Lancet, JCI, PNAS Blood, ATVB, Circulation, and JTH.